The landscape of the cardiac intensive care unit (CICU) has evolved significantly over the past 50 years, owing to the rise in the use of cardiac devices, substantial increases in illness severity, and the need for non-cardiac procedures.1 Initially conceived for the management of acute MI and post-cardiac arrest care, the contemporary CICU has evolved to accommodate care for a more complex patient population characterized by advanced age, increased multimorbidity, multi-organ failure, and non-cardiac critical illness.2 Despite significant advances in CICU care, overall hospital mortality for patients admitted to the CICU remains high – approaching 10% – with approximately half of these patients dying in the unit.3 Finally, a significant proportion of CICU patients receive aggressive or life-sustaining therapies during their stay.3
In this context, shared decision-making (SDM) – a process by which patients and clinicians reach a mutually approved decision about the direction and goals of medical care – in the CICU is essential, in particular for decisions pertaining to palliative or end-of-life care.4
Although SDM is supported by both cardiology and critical care societies, there remains a lack of understanding of what SDM is, when it should be used, and approaches and strategies for promoting SDM in the CICU.5,6
The aims of this review are therefore to: define the fundamentals and models of SDM; describe the role of SDM in the CICU; and describe the available evidence on interventions to promote SDM in the CICU. An improved understanding of SDM in the CICU will contribute to more tailored, patient-centered, and humane care across the spectrum of critical illness.
Shared Decision-making: Fundamentals and Models
SDM is a model of treatment decision-making in which patients and clinicians work collaboratively within clinical practice to establish treatment plans.4 While most models of clinician-patient communication, including serious illness conversations, focus on eliciting patient values and subsequently conveying information to the patient, SDM requires two-way communication to develop a collaborative care plan. The core of SDM is a balance between patient and family autonomy and clinician expertise to create personalized, evidence-based decisions.7 The goal of this process is to encourage individualized patient care tailored to specific preferences and to increase patients’ trust in the healthcare system.
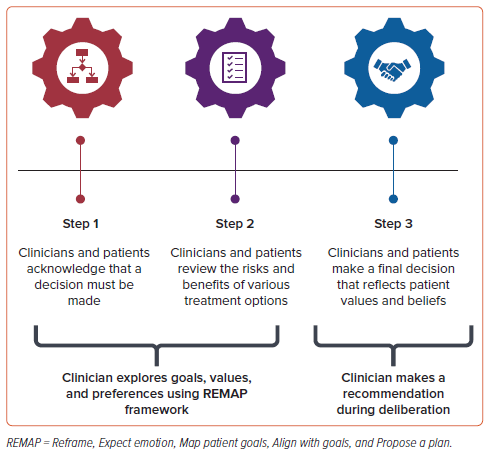
While a number of models and frameworks for SDM have been proposed, the majority have three essential elements (Figure 1).7 First, both parties must recognize and acknowledge that a decision must be made. Then, both groups should understand the best available evidence regarding the decision, including the risks and benefits of the available options. To fully optimize this step, clinicians must possess both knowledge of the data and the ability to share that information in language that is adapted to the patient’s health literacy and communication preferences. Finally, clinicians and patients should work together to make a final decision that reflects the patient’s values, beliefs, practices, and personal goals. Central throughout this process is open communication between clinician and patient via active participation by all parties as joint collaborators with bidirectional sharing of information. Equal weight should be given to the clinical recommendation and the patient’s principles, and each party should seek to gain a better understanding of the other.
Box 1: Clinical Vignettes
Clinical vignette 1: Ms G is a 90-year-old woman with history of coronary artery disease, Alzheimer’s disease with dementia, stage 3 chronic kidney disease, and heart failure with preserved ejection fraction, who presented to the cardiac intensive care unit with cardiogenic shock and acute renal failure due to severe low-flow, low-gradient aortic stenosis. She also has moderate aortic insufficiency. A balloon aortic valvuloplasty is being considered but is deemed high risk given her acute and chronic comorbidities.
Clinical vignette 2: A 38-year-old man with a long-standing history of nonischemic cardiomyopathy presents with heart failure–cardiogenic shock that is unresponsive to medical therapy with IV inotropes. The multidisciplinary heart failure team feels he would benefit from a percutaneous left ventricular assist device as a bridge to heart transplantation or durable left ventricular assist device.
Clinical vignette 3: An 85-year-old man with metastatic non-small cell lung cancer, stage 5 chronic kidney disease, and heart failure with reduced ejection fraction due to ischemic cardiomyopathy presents with a non-ST segment elevation MI and persistent chest pain. An urgent coronary angiogram is considered in the context of his kidney disease and previously expressed desire to avoid hemodialysis.
Other slightly varied models or paradigms for SDM have been promoted. In the three-talk model, clinicians walk patients through a three-step process to facilitate decisions: choice talk, in which the clinician articulates that there are multiple choices but no ‘right’ choice; option talk, in which various options are discussed and compared, using risk communication principles; and decision talk, in which a decision is reached that reflects both the goals and values of the patient and the expertise of the healthcare team.8
Integral to all of these frameworks is an understanding of a patient’s goals and values so that clinicians can make a recommendation that is aligned with patient priorities. From the palliative care literature, a common framework for exploration of goals and values is REMAP: Reframe, Expect emotion, Map patient goals, Align with goals, and Propose a plan.9 In particular, full exploration of the patient’s goals and values (the Map patient goals component) is a critical component of SDM to ensure that the choices offered are explained in relation to those goals. Through incorporating REMAP into SDM, clinicians can help process and understand the various treatment options and their likelihood of providing benefit, assist patients in outlining their hopes, goals, and priorities, and then use their knowledge of these two domains to provide a recommendation (Figure 1). Although many feel that SDM should be a partnered process in which clinicians and patients come to a stated decision together, the formulation of a clinician recommendation is essential to help guide patients in their decision-making.10
Traditionally, patients are asked upfront about role preference, e.g. whether they want to make the decision or defer to a loved one or medical team. However, more recent consensus suggests that the decision-maker be identified after the options and trade-offs have been discussed so that the patient can determine the appropriate decision-maker after they have received all of the relevant information.11 For example, in a study of patients with prostate cancer, many patients who upfront indicated they wished a professional to make the decisions were later found to prefer to decide themselves after having been presented with the information.12
The process of SDM does not end with the conversation. Documentation and dissemination of patient preferences are required to ensure that other members of the patient’s care team can understand and support the care plan. Standardized processes for SDM documentation allow for easy discovery within the medical record, avoidance of repetitive conversations with patients, and enhanced research on SDM impacts on outcomes.
Cardiovascular Disease and Intensive Care Guidelines and Practice
Introduced for the first time in the literature in 1972, SDM is now widely recognized as an ideal approach to patient care by multiple medical disciplines. In the field of cardiovascular diseases, the use of SDM has been studied and promoted across a number of conditions and decisions, including in AF, cardiac imaging, valvular heart disease and interventions, and devices and advanced surgical therapies for heart failure (HF). 13–19 Similarly, SDM has been promoted in intensive care units (ICUs), most notably in a comprehensive policy statement from the American College of Critical Care Medicine and the American Thoracic Society.5 The six broad recommendations endorsed by this statement are described in Table 1.
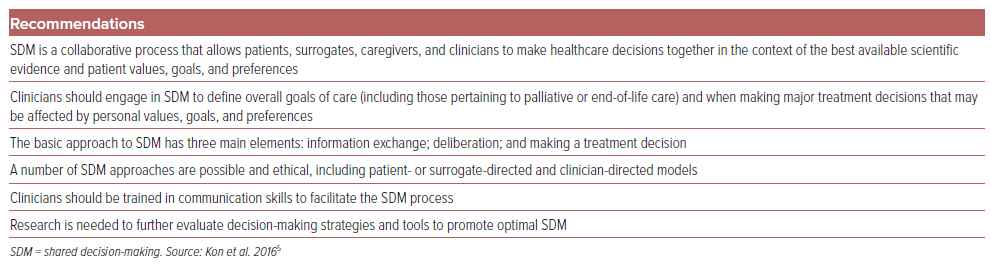
Despite this seemingly widespread recognition of the importance of SDM, gaps still remain. A recent cross-sectional study of 65 cardiovascular guidelines from 2012 to 2022 found only 6% of pharmacotherapy recommendations incorporated SDM in some form.20 Even when SDM is recommended, there is often little guidance as to how to integrate SDM into practice.20 Finally, there are currently no available guidelines or recommendations for SDM in the CICU.
A key issue in SDM is how this approach is incentivized and supported in clinical practice. In 2010, SDM was included in the Affordable Care Act; suggested changes to incorporate SDM into policy included the accreditation of patient decision aids by a national organization, and revisions to procedural terminology codes.21 However, many of these and other changes to incentivize SDM using payment programs have not materialized or have had marginal effects.22 Efforts to shift and incentivize practice towards SDM are still needed.
Palliative and End-of-life Care in the Cardiac Intensive Care Unit: Needs and Barriers
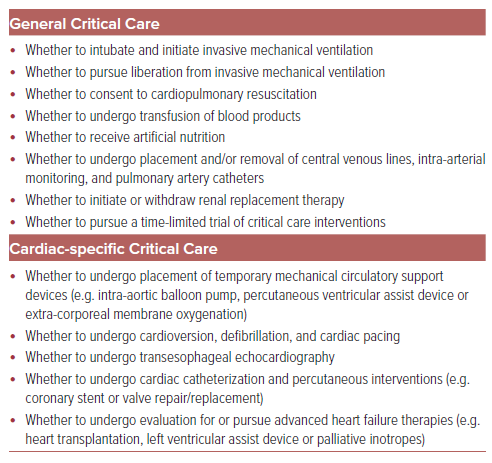
CICU patients experience high mortality and frequently receive aggressive or life-sustaining therapies.3 CICU clinicians and critically ill patients are, therefore, regularly faced with decisions about treatment plans, especially those related to palliative and end-of-life care. These decisions encompass broad goals of care determinations, such as whether to transition to comfort-focused measures, as well as discussions about whether certain therapies should be initiated or withdrawn based on values and preferences. (Table 2). Optimal SDM has been associated with increased patient and family satisfaction in ICUs, especially for decisions related to end-of-life care.23,24
Despite the benefits, routine use of adequate SDM in practice can be complex. Challenges with end-of-life decision-making are well documented in ICUs, and include value conflicts among stakeholders, physician-family disagreements about end-of-life care, and uncertainty among surrogate decision-makers as to the best course of action.25,26 ICU patients may have varying levels of consciousness or ability to participate in decision-making due to critical illness.
Other clinician-facing barriers include discomfort with or lack of training in communication and difficult conversations, practical barriers (namely time constraints and lack of compensation), and navigating different cultural contexts.27 Furthermore, studies have shown that cardiology trainees in particular receive insufficient communication skills training.28
In comparison to medical ICUs, CICUs involve unique challenges due to the presence of complex and often novel devices and procedures. These elements add another layer of complexity to SDM; as the menu of therapeutic options for CICU patients rapidly expands, it becomes more critical to elicit goals and engage patients in determining the best care plan.
At the very least, barriers to SDM will require multifaceted interventions, including adequate staffing to help alleviate clinician time constraints, changes in billing structure that will incentivize clinicians to adequately perform SDM, and broad educational initiatives to increase confidence and competence in SDM and end-of-life communication.
Evidence-based Strategies
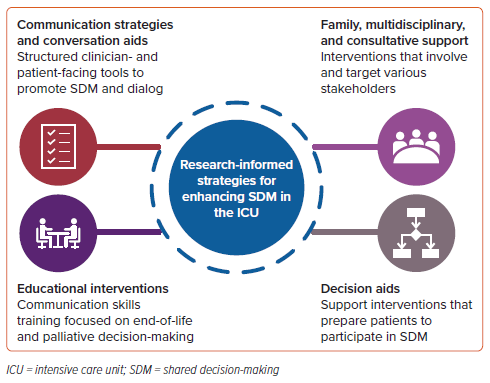
Very few studies have investigated SDM in the CICU specifically. However, a number of strategies to promote high-quality SDM during serious illness and end-of-life care in ICUs have been studied (Figure 2). While these studies are heterogeneous in terms of intervention characteristics, patient population, and outcomes, they all share a common goal of improving the quantity and quality of SDM in the ICU.
Communication Strategies and Conversation Aids
Multiple interventions have been developed that use structured communication tools to enhance communication and promote decision-making in the ICU, albeit with mixed results in trials. In the VALUE (Value, Acknowledge, Listen, Understand, Elicit) communication intervention, a communication mnemonic was used on placards, in daily rounding checklists, and in a templated progress note to prompt ICU clinicians to address values and goals.29 Rates of documented communication improved, with a trend towards an increase in family satisfaction with communication.29
In contrast to these clinician-facing communication interventions, conversation aids are clinician- and patient-facing tools that are designed to support SDM dialog during the clinical encounter between patients and clinicians. Conversation aids may include brochures, pamphlets, or computer-based tools to promote more effective communication during a clinical encounter.30 Many of these interventions have been shown to enhance the quality of ICU communication and decision-making, lessen the burden of bereavement, and decrease the time to decision-making.31–33
Decision Aids
Decision aids are decision-support interventions that have been developed to increase informed choice across a range of health decisions, including in the ICU. In contrast with conversation aids, decision aids can be used outside of the clinical encounter (i.e. before or after an appointment) to assist patients to make decisions.34 Decision aids aim to provide patients with relevant information, improve knowledge, and encourage their involvement in decision-making. Unlike conversation aids, they indirectly prepare patients to participate in SDM conversations with their clinicians, rather than support the SDM conversation itself.
In a study of patients undergoing prolonged mechanical ventilation in three ICUs, a decision aid that aimed to promote SDM about whether to provide continued prolonged life support was feasible, acceptable, and associated with improved decision-making quality and less resource use.35 Other studies of decision aids have demonstrated favorable results in alternative end-of-life decisions (e.g. physician orders for life-sustaining treatment, advance care planning in cancer, and consideration of hemodialysis) or high-stakes decisions for patients with cardiovascular diseases (e.g. left ventricular assist devices and major cardiac surgery).36–40 However, no decision aids have been developed specifically for the CICU population.
Involving Family, the Multidisciplinary Team, and Consultative Support
Various ICU interventions have targeted different stakeholders with the aim of improving ICU SDM. For example, ICU rounds are considered a key opportunity for enhancing decision-making. Studies have shown that inviting the patient and surrogate and/or family members to participate in daily rounds may foster trust and understanding and improve communication between clinicians and patients.41,42 Including other members of the healthcare team in daily rounds may also enhance communication and decrease conflict both within the clinical team and between the clinical team and patient/family.43,44 In particular, communication interventions that target family members and caregivers appear to have potential to improve outcomes, including the quality of SDM and ICU length of stay.45
Studies have also investigated whether the involvement of consultative services with expertise in communications skills and SDM (e.g. palliative care and ethics specialists) is associated with improved communication and decision-making. In a multicenter randomized controlled clinical trial in four medical ICUs, structured family meetings led by palliative care specialists did not reduce anxiety or depression symptoms among family members, and there was no effect on select patient, resource, or decisional outcomes.46 Other studies evaluating the effects of palliative care consultation in the ICU have not consistently shown associated improvements in the perceived quality of dying, satisfaction with care, or depressive or anxiety symptoms, although consultation may be associated with earlier and more frequent ICU family meetings, as well as shorter hospital lengths of stay.46–48
Research has also examined ethics consultation and decision-making in the ICU.49–51 Although outcomes did not focus on decision quality, three studies found ethical consultation was associated with a shorter length of stay, and was variably associated with reductions in life-sustaining treatments. Further studies are needed to determine the optimal characteristics of palliative care and ethics interventions that may improve communication, decision-making, and outcomes.
Educational Interventions
Multiple educational interventions have been developed to enhance the quantity and quality of SDM in the ICU. Primarily focused on medical trainees, a few small studies have shown that educational programs focused on SDM and communication are feasible, satisfactory, and may increase comfort with communication among clinicians.52,53 However, the impact on clinical skills, behaviors, and patient or SDM outcomes is less clear.
There has been considerable interest in enhancing critical care training for cardiovascular medicine physicians, including through integrated or hybrid training programs, as well as a desire to define clinical competencies for the critical care cardiologist.54 Expertise in SDM should be a core competency for the critical care cardiologist. Furthermore, training in communication skills and SDM should feature prominently in all critical care cardiology curricula to arm the next generation of cardiologists with the knowledge and skills to provide optimal patient-centered care in the CICU.
Conclusion
Complex decision-making is commonplace in today’s CICU, owing at least in part to escalating patient comorbidity and illness severity. Although equipped with an evolving and expanding armamentarium of therapeutic tools with which to deliver contemporary critical care, CICU clinicians are nonetheless challenged by patients with greater medical complexity than in previous decades.2
The concept of SDM – in which healthcare decision-making involves a collaborative process between patients, families, surrogates, and clinicians – has been increasingly promoted in general ICUs; its introduction into the CICU context, however, has been limited to date. Therefore, there is a compelling need to both increase awareness and develop the necessary processes to integrate and evaluate SDM in critically ill cardiovascular populations. This will include initiatives to enhance education and training, to identify key obstacles, and to create novel methods for generating evidence. Key stakeholders in the CICU, likely in partnership with experts in palliative care, will be responsible for answering fundamental questions around SDM that include: how to define SDM; how best to employ SDM practices; how to study SDM; how to overcome barriers to its implementation; and how to prove value in this specific patient setting.