True coronary bifurcations (Medina 1,1,1 and most of 1,0,1 and 0,1,1) with side branch (SB) diameter of >2.25 mm and lesion length of >10 mm are likely to require two-stent treatment techniques (Figure 1A).1,2 The Crush technique underwent a series of technical iterations and modifications by Chen et al. before evolving into the so-called mini double kissing Crush (DK-Crush) technique.3,4
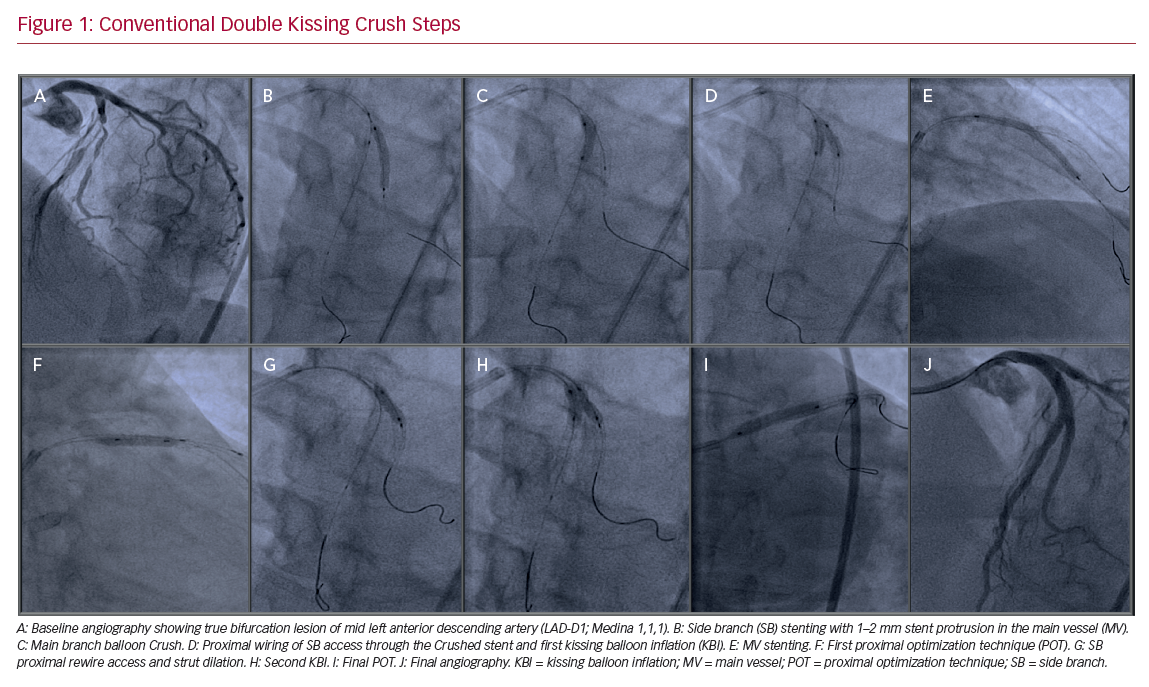
The conventional DK-Crush includes the following steps after adequate lesion preparation:
- stenting the SB (with 1–2 mm protrusion in the main branch (MB);
- removal of SB wire and balloon and MB balloon Crush;
- proximal wiring of SB access through the Crushed stent and first kissing balloon inflation (KBI);
- main vessel stenting;
- first proximal optimization technique (POT);
- SB rewiring access and strut dilation;
- final KBI; and
- final POT (Figure 1).
The main difference between classic and DK-Crush is the use of the first KBI after balloon Crush of the implanted SB stent. Therefore, after MB stenting, one layer of metal struts remains at the ostial SB to cross through, which facilitates the second KBI. Contrary to the provisional SB stenting approach, where guidewire recrossing is suggested to be performed through the distal cells, the first recrossing of the SB during DK-Crush should be carried out through the most proximal cell to avoid malapposition of the SB stent at the carina.4 Compared to the provisional treatment, DK-Crush is superior to the classic Crush and Culotte strategies, because it leads to higher rates of successfully performed final KBI and to lower target lesion revascularizations (repeat interventions), as shown in the DK-CRUSH I, II, III, and V studies.5–8 This led to a class II recommendation for DK-Crush to be used as a treatment option for distal left main bifurcations in the European Association for Cardio-Thoracic Surgery/European Society of Cardiology guidelines.9
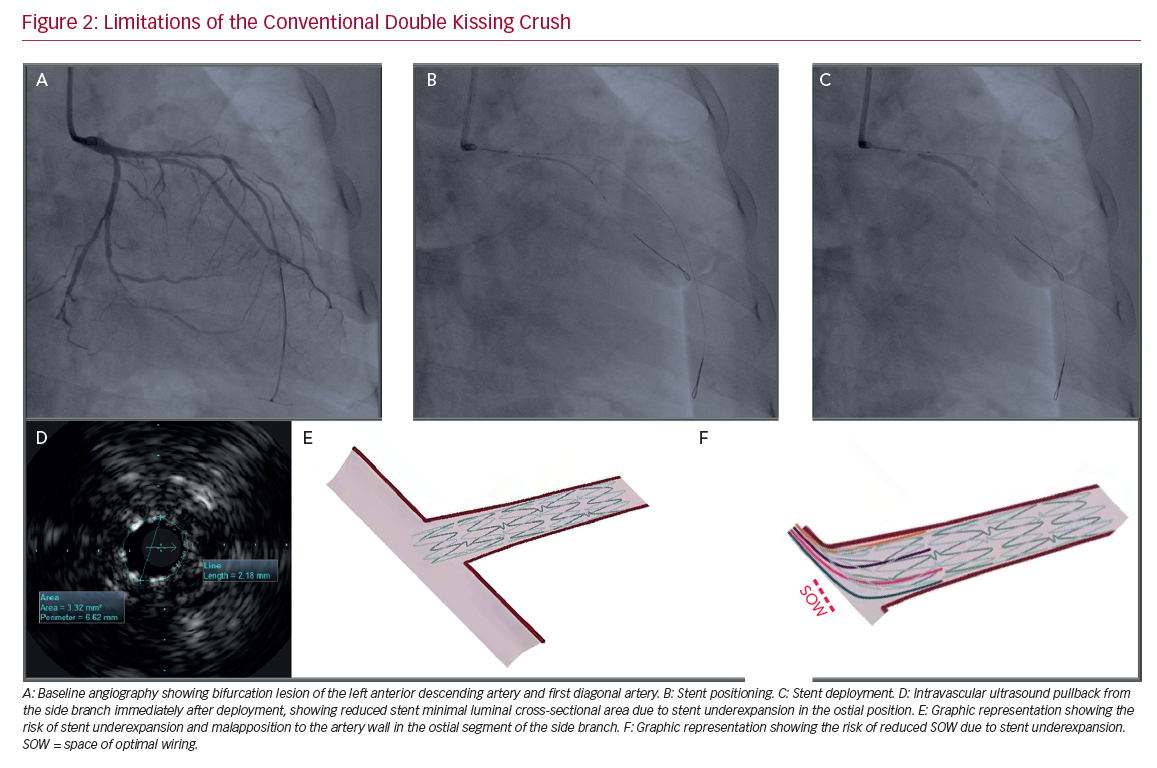
All Crush techniques have the limitation of the inappropriate guidewire crossing in the Crushed SB stent. When this occurs, the SB stent may be further Crushed, leaving the ostium uncovered. Furthermore, it yields difficult SB rewiring after MB stent deployment, and potentially negates the benefit of the Crush technique, leaving the SB ostium uncovered (Figures 2A–2D). KBI may maximize SB access, but is unlikely to optimize SB stent apposition in the para-ostial segment.
The Proximal Side Optimization Technique
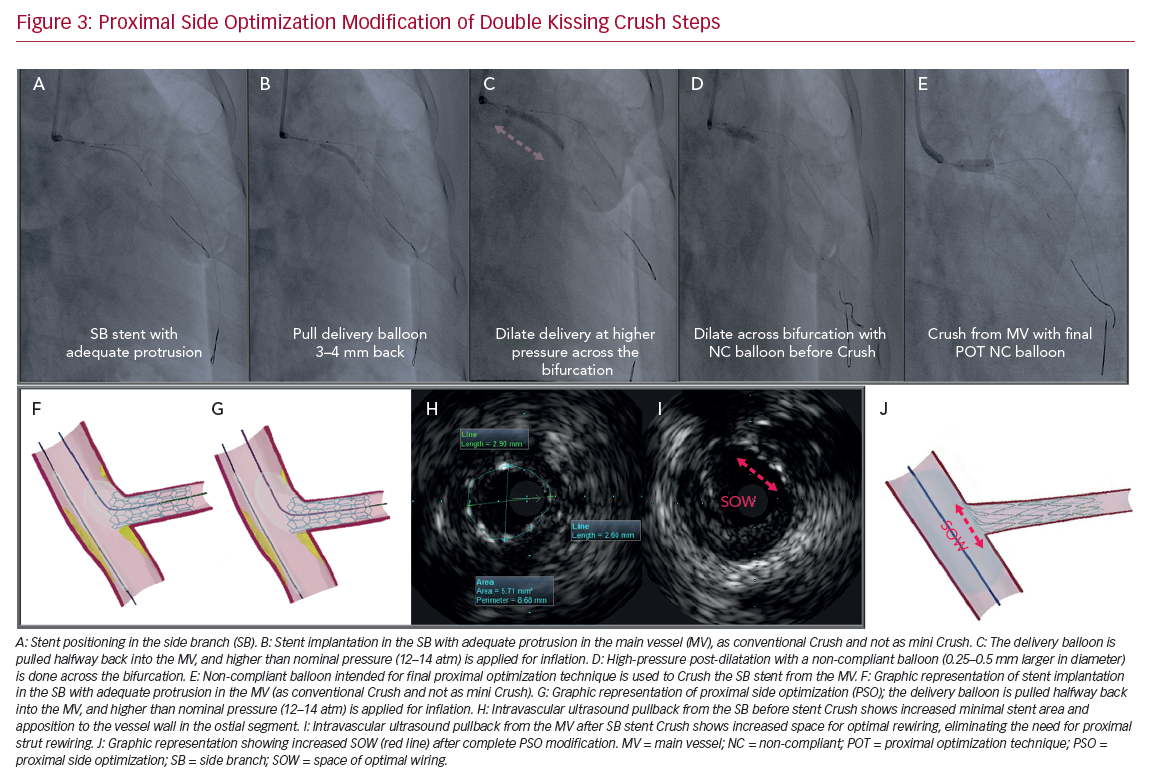
We suggest a small modification to the established DK-Crush technique proposed by Chen et al.,4 which we call the proximal side optimization (PSO) technique. As the SB stent is sized based on the distal reference SB diameter, in long lesions there will be a definite size mismatch with the ostial SB diameter, thus it should be positioned and deployed with adequate protrusion in the MB (as conventional Crush and not as mini Crush; Figures 3A and 3B). In this way, the segment of SB stent is reliably Crushed and completely bent in only one direction in front of the SB, leaving one single layer of the stent struts to be further crossed by the guidewire and opened by the SB balloon (Figure 3H). The delivery balloon needs to be pulled back partially in the MB and deployed at a higher pressure (usually 4–6 atm above ‘nominal’ pressure; Figure 3C). Subsequently, high-pressure dilatation with a non-compliant balloon (0.25–0.5 mm greater in size, or if intravascular ultrasound or optical coherence tomography is used, according to the dimensions of the proximal SB) is performed (Figure 3D). The SB stent is then Crushed from the MB using a big, short, high-pressure balloon designed for final POT (Figure 3E). The rest of the procedure follows the standard DK-Crush technique previously described.
In our experience, the PSO leads to more reliable and considerably easier rewiring of the Crushed stent, most often increasing the area of optimal rewiring (space of optimal wiring, which is smaller before PSO, as with conventional DK-Crush [Figure 2F], and much larger after PSO [Figures 3I and 3J]), and by using the original workhorse soft-tipped guidewire in almost all of the cases. Notably, our modification excludes the necessity to rewire through the most proximal strut, which is discouraged in PSO to avoid the need to pass more layers of stents Crushed there. Similarly, in most cases, after first rewiring we utilize the same non-compliant balloon previously used for high-pressure SB stent post-dilatation to perform the KBI.
Conclusion
The PSO modification ensures stent size ‘accommodation’ to the larger vessel diameter in the proximal segment and better strut apposition to the wall, which are particularly important in the ostial segment where size mismatch between proximal and distal SB dimensions in long lesions is greater (Figure 2E). It can be helpful in all Crush techniques and also in other stent techniques, such as T and protrusion (TAP) and Culotte.
Further serial clinical studies of optical coherence tomography, and bench tests of micro-CT and flow dynamics, need to be performed to demonstrate whether this iteration leads to optimal flow conditions in the carina, further reducing revascularization rates triggered by the restenotic process in the SB ostium.