The specialty of pregnancy and heart disease (or cardio-obstetrics) has established itself as an important sub-specialty in cardiology and maternal medicine. Although covering all cardiovascular disease in pregnancy, most patients attending specialty cardio-obstetric antenatal clinics have congenital heart disease (CHD), at least in high-income countries.1
It is imperative that multidisciplinary teams consisting of experts in the field of adult CHD (ACHD), maternal medicine obstetricians, and specialist anesthetists are available to ensure patients are equipped to make decisions regarding their pregnancy plans and to best support them through the ramifications of these decisions.2 Accurate and reliable risk stratification before and during pregnancy is a vital component of this care.
While pregnancy outcomes in women with CHD vary greatly, having a congenital heart lesion increases the risk of cardiac, fetal, and obstetric complications during pregnancy.3 Pregnancy induces several potentially challenging hemodynamic and physiological changes in women with normal hearts. Therefore, in the presence of CHD, these changes can result in significant maternal, and/or neonatal morbidity and mortality.4
In most women with CHD, pregnancy is generally well tolerated and uneventful. However, the risk of adverse outcomes depends on a wide variety of risk factors based on the various aspects of the patient’s health profile. To date, most risk stratification tools have focused on the cardiac risk predictors and cardiac events.
Current Cardiac Risk Stratification Tools
The pre-existing risk stratification tools have been a real step forward in the care of these patients and are used by most practitioners in this field. The various scores use different methodologies and were developed in different populations, although the majority of these were high-income countries.
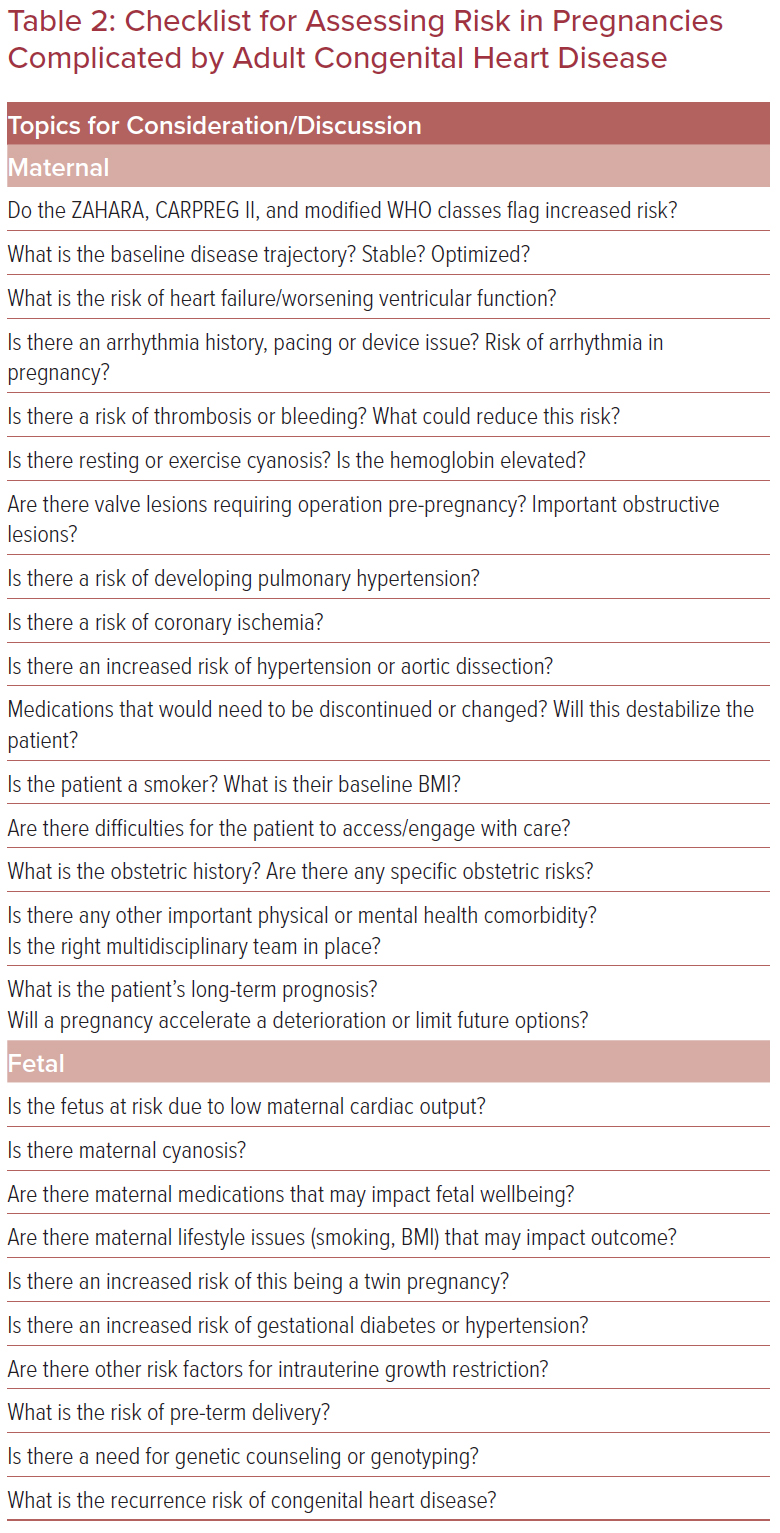
The first widely used model to assess maternal risk was the original CARPREG risk stratification tool published in 2001.5 This Canadian-based study was derived from prospectively collected data on maternities in patients with cardiac disease. CARPREG identified four equally weighed predictors assigning a score of 0, 1 or >1 points. This translated to a 5%, 27% and 75% risk of maternal cardiovascular adverse events, respectively. The ZAHARA risk stratification tool was derived from the Dutch ACHD population. It allocates a weighted score for eight predictors. The final added score between 0 and >3.51 translates to a maternal cardiovascular event rate of 2.9–70%.6 The benefit of the ZAHARA risk stratification tool is that it is ACHD specific. CARPREG II included the original four predictors but additionally incorporates lesion specific and process of care predictors to give an overall sum of 0, 1, 2, 3, 4, or >4 points corresponding to an event rate between 5 and 41% (Table 1).7
The modified WHO (mWHO) risk stratification tool 2011 was based on expert consensus categorizing maternal cardiac lesions into five categories according to ascending maternal risk.4,8 These groups do not have a numerical weight and therefore are not technically a risk score. The mWHO scale is the leading lesion specific stratification tool. In the 2018 European Society of Cardiology guidelines, the five categories were updated to include other aortopathies and coronary artery disease.2
Comparison of the Risk Stratification Tools
Several studies have compared these tools, although, as mentioned above, they were derived from different populations with different outcome definitions. In a comparison of predicted risk versus observed risk, the following results were established: 10.1% versus 4.0% for CARPREG, 8.6% versus 5.0% for CARPREG II, 11.1% versus 8.0% for ZAHARA, and 12.4% versus 8.0% for the mWHO classification. In this study, the ZAHARA model was concluded to be the closest predictor of maternal risk in CHD patients.9 In another study of 3,426 pregnancies with CHD, the ZAHARA risk stratification tool and the mWHO classification performed similarly well, slightly ahead of the original CARPREG tool.10 (This study pre-dated CARPREG II). Other authors have suggested the mWHO is superior.11,12
More recently, the Canadian Cardiovascular Society described the CARPREG II risk tool as having a superior predictive accuracy over the mWHO classification and CARPREG I.13 Conversely, the mWHO is largely still regarded as the simplest to apply clinically. The mWHO classes were used in the large multicenter worldwide cohort studies from ROPAC, in which the majority of the patient population had CHD.14
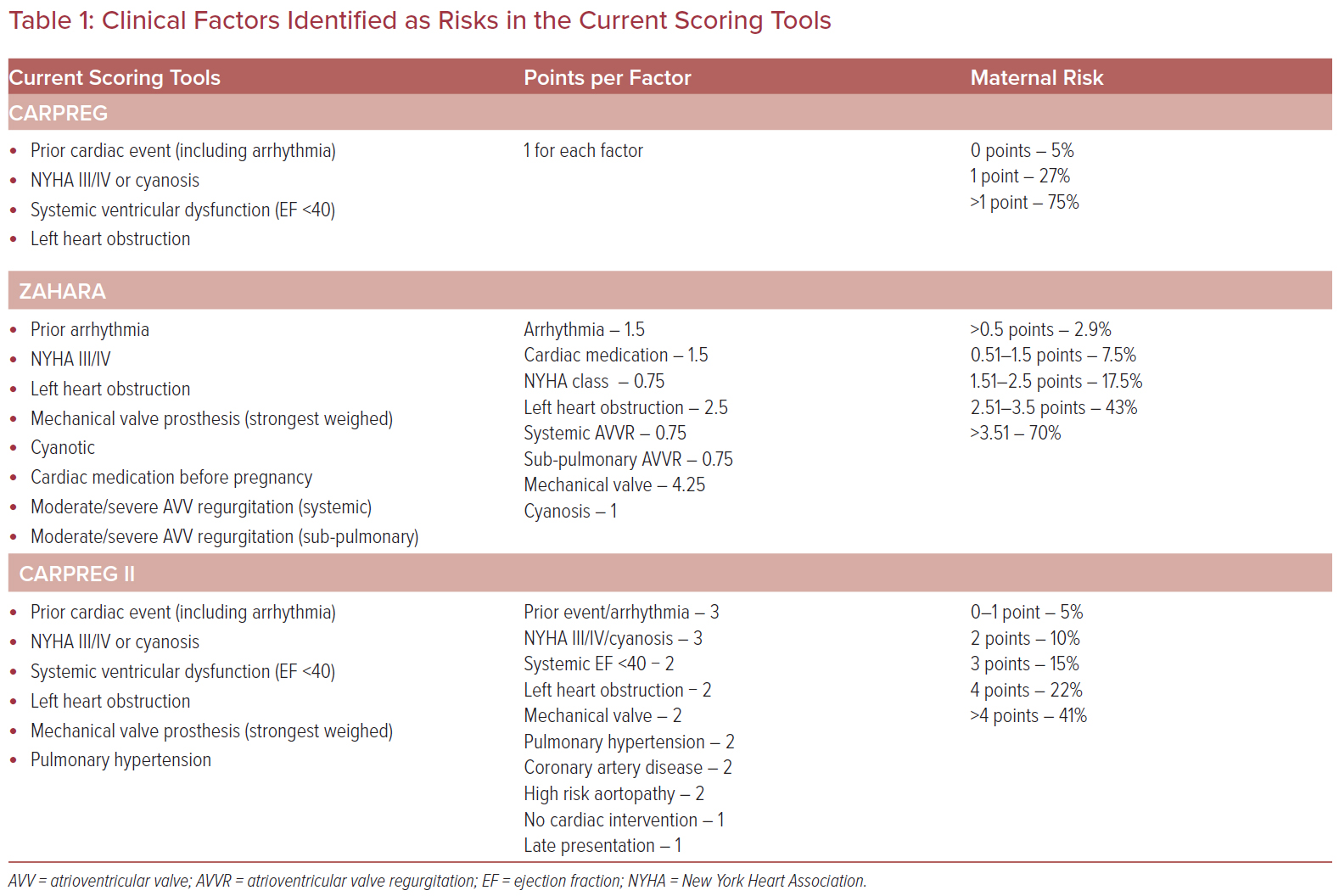
In the recent Canadian Cardiovascular Society guidelines, a more pragmatic approach was proposed. This suggested flagging the high-risk mWHO patients and then using CARPREG II to stratify these patients into low- and intermediate-risk groups (Figure 1).13
In terms of the whole cardio-obstetric population, most women who die of cardiac disease in pregnancy were not known to have a cardiac condition.15 This is a rare occurrence in CHD and, therefore, women should, at least in theory, have access to pre-conception counseling and expert multidisciplinary pregnancy care. Maternal mortality from CHD is rare, but it is not clear how much of this is due to early assessment and expert multidisciplinary care.
Although these risk scores tend to overestimate risk in the more complex patients, it should be remembered that these risk scores are often derived from data sourced from expert centers. There are several real-world examples where the actual outcomes are poorer than in registries, for example complications related to mechanical valves.16
Missing from the Risk Scores
No risk tool can have the granularity needed to fully assess an ACHD patient planning pregnancy. For example, no two Ebstein patients are the same. The subtleties of their individually balanced circulations do not come out on any of the traditional risk scores. In addition, there is little to clarify about how to combine risks, for example the patient with a small and relatively ‘stenotic’ mechanical mitral valve prosthesis, placed when the patient was a child: do two mWHO III lesions add up to group III or IV?
As risk scores are often based on population data, the risks associated with rare diseases are often overlooked. For example, severe pulmonary hypertension does not come out in all the points-based risk scores, and conditions such as Ebstein’s anomaly are not seen in the mWHO classes. Therefore, the absence of a high-risk score does not equate to the absence of risk.
Most of the recognized non-cardiac risk factors (except late presentation in CARPREG II) were excluded from the risk scores. These non-cardiac issues are often the final insult to a borderline clinical situation and can be the trigger for adverse events. Maternal obesity, smoking, ethnicity, and age are all known to increase the risk of cardiac death.17 Logistics of care and inability to engage with care can elevate risk considerably. This includes lack of access to timely specialist care, distance from specialist center, psychosocial disadvantage, and language barriers.
It is vitally important that the maternal medicine and obstetric teams are involved in pre-pregnancy or early pregnancy risk stratification. This allows for a more comprehensive assessment of risk and gives patients early access to treatment that may modify risk, such as aspirin for pre-eclampsia.
Fetal Risk
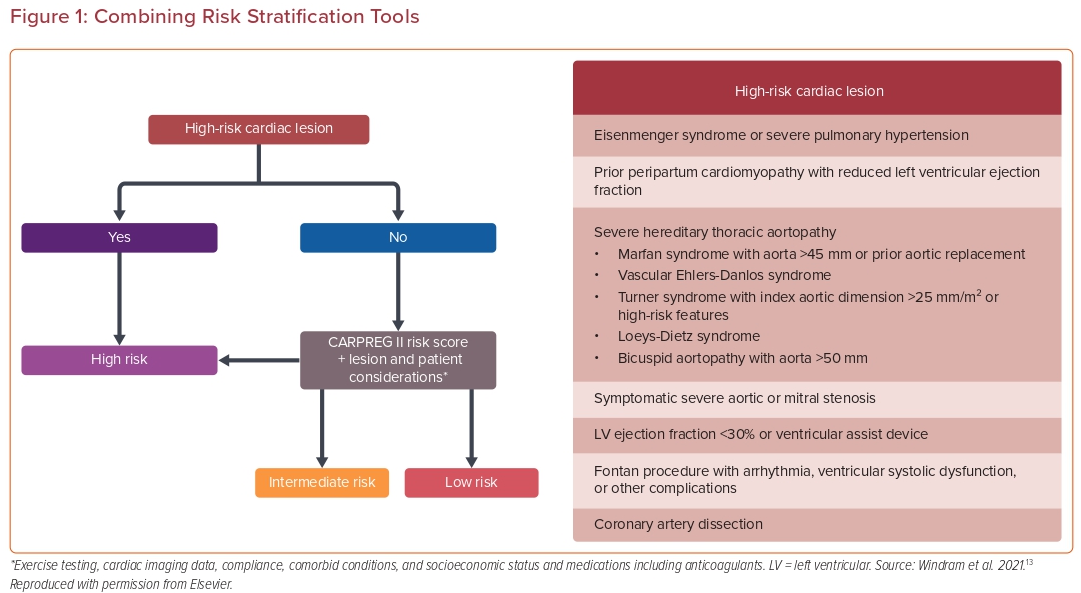
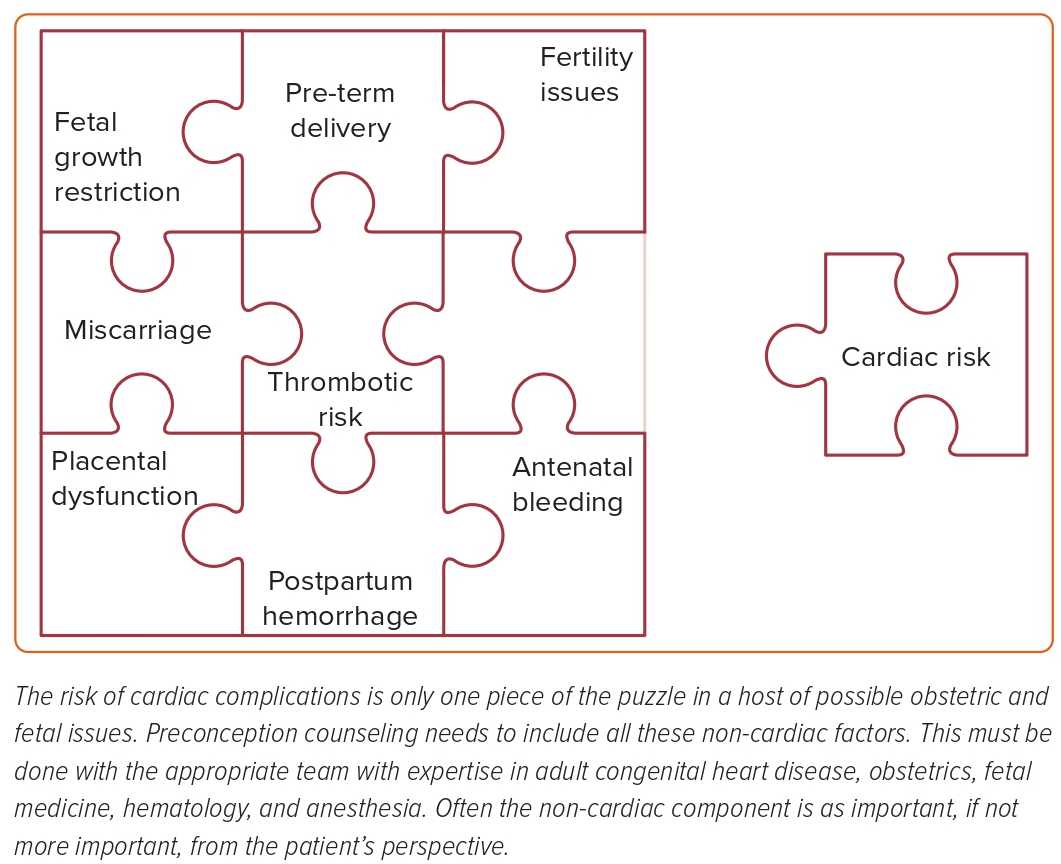
Although perinatal mortality observed in pregnancies with CHD is still relatively low at 2–4%, these risks are higher than in the non-ACHD population. Important fetal morbidity occurs in 16–18% of pregnancies and is even higher in certain conditions (Table 2).5 Low birth weight and prematurity may have more profound consequences for the neonate and its family than a limited treatable maternal cardiac complication and it is frequent for pregnant women to selectively accept more personal risk in the belief that it will minimize fetal risk (e.g. choosing low molecular weight heparin over warfarin for mechanical valves). The recurrence risk of the fetus having a congenital heart condition should not be forgotten and these women should be offered routine fetal echocardiography.
Non-cardiac Adverse Events
These risk tools focus on maternal cardiac complications. In many congenital lesions, such as a Fontan circulation, the risks of obstetric and neonatal risks outweigh the specific cardiac issues (Figure 2).18 Although heart failure and arrhythmia are significant challenges for these patients’ fertility, recurrent miscarriage and increased risk of fetal death are the events that patients fear the most. Women with ACHD should undergo pre-pregnancy counseling that includes all these other factors. This may result in a long complex consultation or the need for several discussions.
The Patient Perspective
The journey for the patient is not viewed solely through the lens of cardiac risk. The patient’s whole pregnancy story includes issues around fertility, miscarriage risk, wellbeing during pregnancy, logistic consideration, delivery stories and fetal outcomes. To the patient, all complications are not considered equal. A patient with, for example, a Mustard operation with recurrent arrhythmia will view a readmission for cardioversion (something she may have experienced many times before) very different from per vaginal bleeding, a new experience that may lead to severe anxiety regarding fetal loss.
Clinical Example
JL was born with transposition of the great arteries and had a Mustard repair in early life. She feels well, but is relatively inactive. She has never had heart failure or arrhythmia. She is on no medication. Her echo shows good systemic RV function but there is significant tricuspid regurgitation. There is also a baffle leak with mild volume loading of the left ventricle. Her oxygen saturations are normal. She is contemplating pregnancy.
JL’s risk of maternal cardiac event is:
- ZAHARA score – 0.75 points for AV valve regurgitation. Risk of 7.5%.
- mWHO class – Group III as systemic RV. Risk of 19–27%.
- CARPREG II – 0 points. Risk of 5%.
JL is 41 years old and an ex-smoker. She lives about 80 miles from the nearest specialist center. She does not drive, but her partner does. She had a previous pregnancy 3 years ago complicated by gestational diabetes and significant intrauterine growth restriction. She required delivery by cesarean section at 34 weeks for fetal indications. She currently weighs 110 kg and has a BMI of 39.1. None of these additional factors add to the cardiac risk scores, but do significantly add to the complexity of care and to risk.
Other Ways of Assessing Risk
Previous pregnancy history is a rich source of additional information in terms of risk. This is especially true for obstetric complications and for information regarding delivery. In patients with CHD, anatomical and physiological findings tend to change slowly. Therefore, a previous uneventful pregnancy 2 years prior is often, although not inevitably, a reassuring finding. A previous straightforward vaginal delivery greatly increases the chances of a further successful vaginal delivery.
As in other circumstances, there are many other tools used to estimate risk in ACHD patients. They include parameters of exercise performance on testing such as heart rate reserve, peak oxygen uptake and biomarkers, such as BNP.17–19 Stress echo and stress MRI can be useful adjuvants when assessing functional reserve. Early discussion around pregnancy, ideally several years before the patient is planning a pregnancy, gives time for full assessment and maneuvers to optimize cardiac function.
Long-term Outcome
The risk scoring systems all focus on the short-term risk of cardiac events. Equally important are the long-term implications of a pregnancy on cardiac status. There is particular concern regarding the impact of pregnancy on ACHD patients with ventricular dysfunction, aortic dilatation, and elevated pulmonary artery pressures. Again, this is a nuanced discussion and requires expertise, especially in areas where there are limited data. The impact of pregnancy on issues such as future transplant options should also be included in any discussion with a complex patient as pregnancy may produce sensitizing antibodies that reduce a patient’s chances of receiving a donor heart.
Conclusion
The traditional risk scores are excellent at flagging patients at risk. However, they are only a starting point for pre-pregnancy and early pregnancy counseling. A more nuanced conversation, in a multidisciplinary environment, is required for all but the simplest of CHD lesions. These are often long and detailed discussions requiring the clinical team to have both an awareness of the literature but also comprehensive experience and expertise in cardiac, obstetric, anesthetic and neonatal care. For this reason, patients with ACHD should be referred to an expert cardio-obstetric clinic for pre-pregnancy planning. A checklist of points for discussion or tables of red flags may facilitate these conversations. 











Comments