Background: The most widely known risk factors for stiff left atrial syndrome are catheter ablations and maze procedures for atrial fibrillation. Here, we describe a rare case of a stiff left atrial syndrome years after radiotherapy for breast cancer.
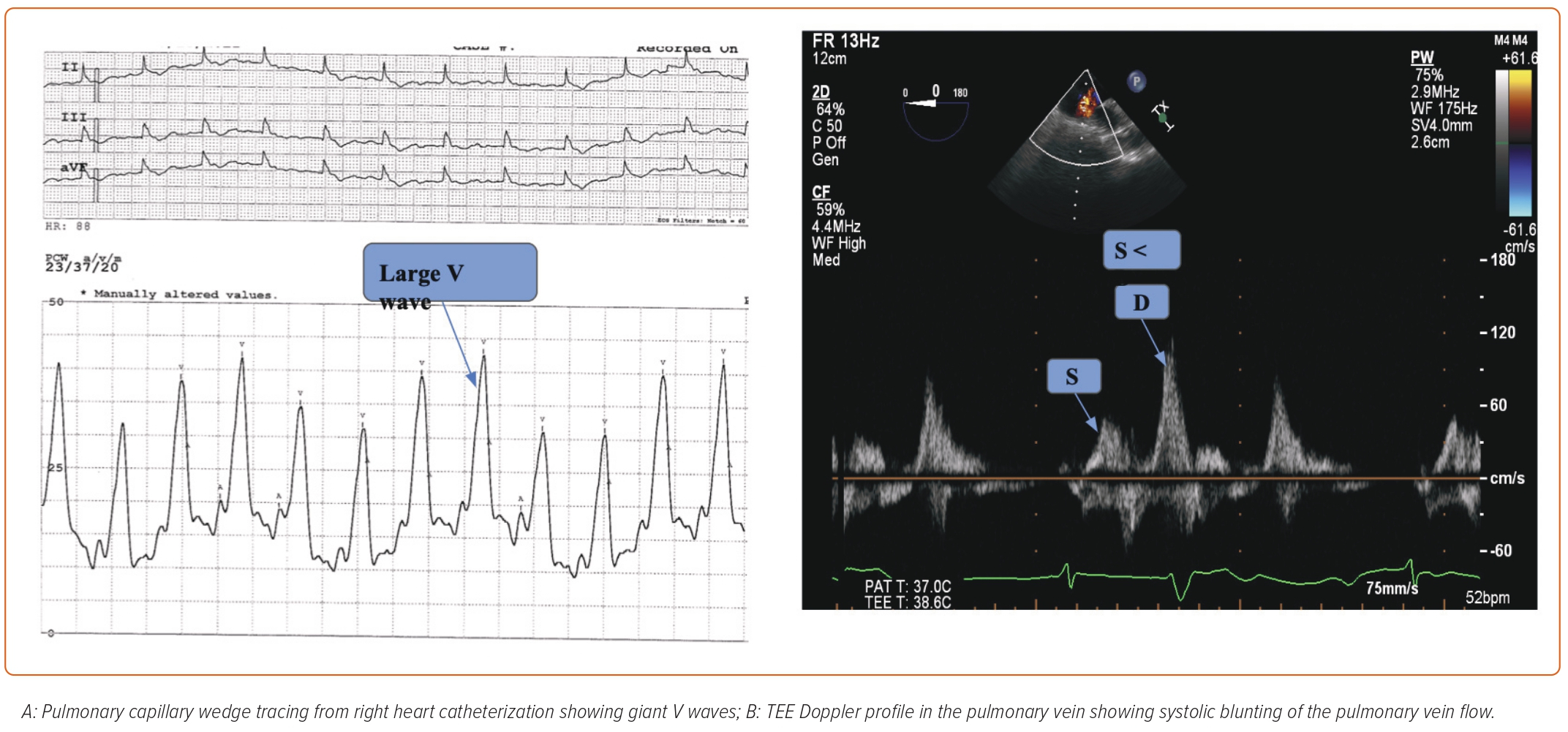
Methods: A 68-year-old female with permanent atrial fibrillation and a history of radiotherapy for right breast cancer presented with worsening isolated dyspnea on exertion. Transthoracic echocardiogram showed severely dilated right and left atrium. A right heart catheterization was performed that demonstrated moderate pulmonary artery hypertension (29mmHg), and pulmonary capillary wedge pressure (52mmHg) with giant V waves apparent on the tracing (Fig 1A). A transesophageal echocardiogram showed no significant mitral regurgitation and the presence of systolic blunting of the pulmonary vein flow consistent with stiff left atrial syndrome (Fig 1B). There was no history of atrial ablation, prior atriotomy, or open heart surgery; hence radiotherapy was suspected as the unique predisposing factor.
Results: In our patient who presented with worsening, effort dyspnea giant V waves on PCWP tracing out of proportion to left ventricular diastolic end pressure and significant mitral regurgitation were indicative of stiff left atrial syndrome after radiotherapy for breast cancer.
Conclusion: Stiff left atrial syndrome is uncommonly associated with radiotherapy and may be an under-recognized etiology of dyspnea in this patient population.