Case
A 60-year-old man has a witnessed cardiac arrest while walking down the street. Bystander CPR is initiated, and emergency medical services (EMS) arrive within 8 minutes.
His presenting rhythm is VF and he is immediately defibrillated. Unfortunately, he remains in VF. Despite 20 minutes of high-quality resuscitative efforts (including five further shocks), he is still pulseless and is transported to your hospital center. On arrival to the emergency room (40 minutes after the initial cardiac arrest), you are asked whether the patient should receive continued conventional CPR or extracorporeal CPR (eCPR). The eCPR team can be ready for cannulation in 10 minutes.
Point: eCPR is Life-saving
This scenario is a familiar one to cardiologists, critical care specialists, emergency room physicians and emergency medical personnel. Until recently, conventional CPR has been the standard of care for these patients, with high morbidity and mortality. However, the use of eCPR to provide immediate and full cardiorespiratory support has demonstrated superior outcomes compared to standard advanced cardiac life support (ACLS). While the application of eCPR continues to be an evolving therapy it deserves strong consideration as part of the management of cardiac arrest in the right circumstances.
The ARREST trial was the first randomized control trial (RCT) to assess the efficacy of eCPR compared to standard of care, ACLS.1 The trial randomized 30 patients with refractory (more than three shocks) out-of-hospital cardiac arrest (OHCA) and initial shockable rhythms. The study was stopped early by the data safety and monitoring board (DSMB) at its first preplanned analysis due to the superiority of eCPR in survival to hospital discharge (43% versus 7%, p=0.023). Survival with neurologically favorable outcomes, as defined by a cerebral performance category (CPC) score of 1–2, was higher with eCPR compared to ACLS at discharge (43% versus 0%), 1 month (43% versus 0%) and 6 months (43% versus 0%), although given the lack of survivorship in the ACLS arm, statistical comparisons were not possible.
The second RCT evaluating eCPR, the Prague study, enrolled 256 patients who had witnessed OHCA with any presenting rhythm without return of spontaneous circulation (ROSC) after 5 minutes of ACLS and randomized them to intent to cannulate for eCPR or standard ACLS.2 The study was terminated by the DSMB because of futility. Survival at 180 days with a good neurological outcome (CPC score 1–2) was not significantly different between groups (31.5% for eCPR versus 22.0% for ACLS; OR 1.63, 95% CI [0.93–2.85]; p=0.09).
While the Prague study appears to refute the findings of the ARREST trial, there are key design differences that may explain apparently different results. First, patient selection for the ARREST trial included only shockable rhythms, which typically have a higher frequency of potentially reversible etiologies compared to non-shockable rhythms (e.g. coronary artery disease).3–5 This aligns with a secondary analysis of the Prague data showing patients with an initially shockable rhythm had better neurologically favorable outcomes at 180 days compared to non-shockable rhythms, both in patients who achieved ROSC prior to arriving at the hospital and in those who were cannulated for eCPR (prehospital ROSC: 69.8% versus 15%; eCPR 33.3% versus 2.9%).6
Second, while the Prague study was designed assuming a 10% survival for the ACLS group, it was more than double what was anticipated (22%). Increased survival was potentially due, in part, to the early randomization, where patients were eligible after 5 minutes of CPR without ROSC (911 call to randomization – ARREST ≈50 minutes versus Prague ≈25 minutes). As such, the benefits of eCPR relative to conventional CPR may have been mitigated by inclusion of an inherently less moribund population. In fact, 36% of patients enrolled in the Prague study achieved sustained ROSC on admission compared to <1% of those enrolled in ARREST. Furthermore, only 66% of those enrolled in the eCPR arm in the Prague study were cannulated (the remainder of patients achieved ROSC), compared to 100% cannulation in the ARREST trial. In one secondary analysis of the overall survival in the Prague data, when patients who achieved prehospital ROSC were excluded, neurologically favorable outcomes at 180 days were superior for eCPR compared to ACLS (21.7% versus 1.2%, p<0.001).6
Third, reviewing the outcomes of patients who crossed over is important. Among those who crossed over from the ACLS to the eCPR group, five of the 11 (45%) survived with neurologically favorable outcomes at 180 days while no patients who crossed over from the eCPR to the ACLS arm had neurologically favorable survival.2 This suggests that appropriately selected patients with truly refractory cardiac arrest have superior outcomes with eCPR compared to ACLS.
Finally, a post hoc Bayesian re-analysis of the Prague trial was performed by the original investigators, demonstrating a neurologically favorable survival at 180 days with eCPR compared to ACLS across skeptical and enthusiastic scenarios.7
The INCEPTION trial was the first multicenter eCPR RCT, enrolling 160 OHCA patients with an initially shockable rhythm and no ROSC within 15 minutes of ACLS.8 Patients were randomized before arrival in the emergency department to eCPR or ACLS. Authors reported no difference in survival with a good neurological status (CPC score 1–2) at 30 days between eCPR and ACLS (20% versus 16%, respectively, p=0.52). Likewise, the serious adverse event rate was the same in both groups (1.4 ± 0.9 for eCPR versus 1.0 ± 0.6 for ACLS).
Like the Prague study, this study had methodological differences from the ARREST trial that may explain their differing findings. First, the cannulation experience in INCEPTION was spread among 10 hospitals and multiple providers. This corresponded with longer cannulation times (start of cannulation to flow – INCEPTION 20 minutes versus ARREST 7 minutes) and substantially longer low-flow time (74 minutes) than was reported in either the ARREST (59 minutes) or Prague (61 minutes) trials.
Second, there was an 11.5% unsuccessful cannulation rate due to complications or failure of circulation, which is very high compared to both the ARREST (0%) and Prague (2%) trials. This issue may be due, in part, to a low number of cannulations per provider team per year (1–2 cannulations/year/institution, 10 hospitals, 52 cannulation attempts, 4-year trial).
Third, the INCEPTION trial had an exceptionally short median stay in the intensive care unit (ICU) for the eCPR group (1 day). Current recommendations are to observe patients post arrest for a minimum of 72 hours before neuroprognostication in the absence of catastrophic neurological injury, making problematic the 43% of patients in the eCPR cohort in whom care was discontinued for neurologically unfavorable survival on day one in the ICU.9
Fourth, of the patients who were cannulated and successfully attained circulation, survival in the INCEPTION trial was lower than in either of the prior two RCTs or the Extracorporeal Life Support Organization (ELSO) aggregate data for eCPR globally (INCEPTION 9.6% versus ARREST 43% versus Prague 31.6% versus ELSO eCPR cohort 20–30%).
Finally, like the Prague study, the INCEPTION trial had a higher than expected survival in the ACLS arm (anticipated 8%; actual 16%) and only 66% of the enrolled patients in the eCPR arm were cannulated and attained circulation.
The INCEPTION trial reveals several key concepts regarding implementing eCPR in a multi-institution setting: special attention is necessary to ensure training and maintaining cannulation skills among providers; consideration for reducing the number of cannulators to improve efficacy may be necessary; exceptionally long time to cannulation (significantly >60 minutes) will likely reduce the survivorship in refractory cardiac arrest patients; and experienced ICU providers familiar with venoarterial extracorporeal membrane oxygenation (VA-ECMO) and post cardiac arrest care should be part of the management team either as primary providers or to assist with protocol development. Of note, even considering these caveats, a recent post hoc Bayesian re-analysis has suggested neurologically favorable survival at 30 days in favor of eCPR at various thresholds.10
While there have been efforts at evaluating the aforementioned studies as part of systematic reviews and meta-analyses, differences in their respective statistical and methodological designs make gross amalgamation of data inappropriate.11–13 Pooled analyses, including patient level data, can begin to unfurl the truth. One such pooled analysis of the ARREST and the Prague studies, including 286 patients with all rhythms, concluded that eCPR cannulated by a highly skilled team of interventional cardiologists serving a larger metropolitan area had better survival at 180 days compared to routine ACLS (32.4% versus 19.7%, p=0.015).14 The effect was larger in patients presenting with shockable rhythms (absolute difference 18.8%, 7.6–29.4; p=0.01; HR 2.26 [1.23–4.15]; p=0.009) and prolonged CPR >45 minutes (HR 3.99 [1.54–10.35]; p=0.005). These data tell a treating physician that for refractory shockable OHCA patients, individuals who receive eCPR in a well-established system with expert operators will derive a 25–33% absolute improvement in survival compared to ACLS (i.e. a number needed to treat of 3–4).
Assessing cost-effectiveness is a difficult task complicated by the fact that once the benefits of an intervention are clear, technological improvements, competition and innovation will tend to reduce costs over time. Despite this, there are several attempts evaluating the cost-effectiveness of eCPR which are well summarized by a systematic review published in 2022.15 The findings demonstrated that for all studies reviewed, eCPR was cost-effective compared to ACLS and estimates the eCPR cost per quality adjusted life year (QALY) is $4,026–$56,156. Cost-effectiveness thresholds are not uniform and remain controversial.16,17 Nonetheless, thresholds published in 2014 range from $50,000 to $200,000 per QALY, suggesting eCPR is cost-effective. It is worth noting that mean annual and lifetime productivity loss per OHCA in 2018 was $48,224 and $638,947, respectively, equating to $11.3 billion annual productivity and $150 billion lifetime productivity losses in the US. This leaves OHCA third among disease processes in terms of productivity loss per annual death and perhaps higher dollar resources should be allocated to combat mortality.
Notably, while the systems of care required to build and maintain an eCPR program are vast, they overlap with other existing therapies and institutional programs. Therefore, these costs may be partially mitigated by engaging and modifying preexisting infrastructure. Examples of this include educating emergency medical providers about protocols and management of cardiac arrest patients, adjusting availability of perfusionists who already facilitate cardiopulmonary bypass, and including ST-segment elevation MI (STEMI) interventional cardiology teams, on-call emergency room, intensivists, or surgical teams as cannulators.
When patients are thoughtfully selected and the care is appropriately and timely administered, eCPR saves lives. Indeed, further research is warranted to understand how to better and more broadly implement systems of care that will allow for effective provision of this life saving treatment. Caution is advised to not conflate the challenge of developing systems of care with appropriateness of delivering care. In summary, eCPR is a life-saving therapy that holds the power to revolutionize cardiac arrest care.
Counterpoint: eCPR is Resource Wasting
eCPR has burst onto the scene, hailed as a breakthrough method of treatment for patients, such as this one presented who had a cardiac arrest. While one small phase II trial has shown that eCPR improves survival, all larger randomized controlled trials have been negative with significant potential for harm. Prior to broad-based implementation of eCPR programs, meticulous understanding of the previously performed trials, in combination with future multicenter RCTs are required to definitively evaluate its efficacy and safety.
The ARREST trial was a single center phase II trial that randomized 29 patients (18–75 years of age) with an OHCA, initial ventricular tachycardiac (VT) or VF rhythm, were refractory to four or more shocks, and had an estimated transport time <30 minutes to either transfer for eCPR cannulation or standard ACLS.1 The study was stopped early by the DSMB at its first preplanned analysis. The primary outcome (survival to hospital discharge) was higher in the extracorporeal membrane oxygenation (ECMO) arm (43% versus 7%, p=0.023). Several design aspects should temper the enthusiasm of the results. As noted, the study was single-centered and enrolled a small number of patients. Moreover, eCPR was instituted by a highly experienced, highly trained cannulation team at one of the largest eCPR centers in the US. Whether these results can be replicated elsewhere remains to be seen.
The Prague OHCA study enrolled 256 patients (18–65 years of age) with a witnessed OHCA and any underlying rhythm without ROSC after 5 minutes of ACLS to intra-arrest transport with mechanical CPR to a catheterization laboratory with the intention of proceeding with eCPR or standard ACLS.2 Contrary to ARREST, this study was terminated by the DSMB because of futility. In this larger cohort, the primary outcome of 180-day survival with a good neurologic outcome (defined as CPC score 1–2) was not significantly different between the invasive (31.5%) and standard group (22.0%) (OR 1.63, 95% CI [0.93–2.85]; p=0.09). There was a trend towards improved outcomes with eCPR among patients with a shockable rhythm, but this was not significantly different (p=0.54). Importantly, there was a signal of potential harm in the eCPR arm with higher rates of bleeding (31% versus 15%), despite limited reporting of other serious ECMO complications such as stroke, mesenteric ischemia, infections, or limb ischemia.
The INCEPTION trial was the first multicenter eCPR trial. INCEPTION enrolled patients 18–70 years of age with an OHCA, an initial ventricular arrhythmia, and who received bystander CPR with no ROSC within 15 minutes of ACLS.8 A total of 160 patients were randomized at 10 centers to intra-arrest transport to an emergency department for eCPR or standard ACLS. The authors reported no difference in the primary outcomes of survival with a good neurological status (CPC score 1–2) between the eCPR (20%) and the standard care arms (16%). In addition, there were more per patient serious adverse events (1.4 versus 1.0) in the eCPR arm including major bleeding, limb ischemia, and cannulation dislodgement. Criticism of technical aspects of this trial points up some of the challenges in establishing a broad eCPR program and in selecting patients for inclusion. Specifically, despite choosing centers in the Netherlands with VA-ECMO experience, cannulation times were longer than expected (low-flow time of 74 minutes) and 11.5% of cannulations were unsuccessful.
These data have since been summarized in a meta-analysis which reported no significant increase in favorable neurological survival at 6 months (RR 1.48, 95% CI [0.88–2.49]; p=0.14), no difference in in-hospital mortality (RR 0.89, 95% CI [0.74–1.07]; p=0.23), moderate heterogeneity between the trials (I2=53%), and no differences in key subgroups.11 Independent groups that have applied the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework to evaluate the evidence for eCPR in these studies have concluded that the overall certainty of the evidence was “low.”12
Finally, the cost of eCPR merits consideration. While studies have reported that the expense of eCPR is €12,254–€155,739 per QALY in observational studies, it is important to note that these include hospital-based costs only and do not include the system, infrastructure, or rehabilitation.12 More importantly, none of the three aforementioned randomized trials have published a cost analysis. This burden is likely to be exponentially larger in smaller hospital systems, wherein there are greater opportunity costs of using limited number of ECMO circuits, and higher intangible costs in the setting of workforce fatigue due to fewer specially trained staff.
In summary, eCPR has only been shown to be beneficial in one small phase II study and larger single and multicenter randomized trials have been negative suggesting that the initial positive results of the ARREST trial cannot be easily replicated in other regions. These trials have also reported important safety signals that should not be overlooked despite limited reported of all potential eCPR. Taken together, the results of existing eCPR trials could be considered hypothesis-generating research and future larger multicenter RCTs are required before strong recommendations for routine implementation can be made by international societies.
Discussion
The incidence of OHCA and in-hospital cardiac arrest (IHCA) in the US is substantial, estimated at more than 350,000 and 200,000 per year, respectively.18 While survival rates for index hospitalizations are poor in patients with IHCA (15–34%), they are even worse in those who experience OHCA (8–10%).18–21 This is compounded by high degrees of functional and cognitive impairment, the development of new medical comorbidities, and poor quality of life.
With the advent and increased use of cardiopulmonary bypass for cardiothoracic surgery in the 1950s, it was suggested that this technology could be extended for the use of CPR in carefully selected patients. In this way, cardiac output (and tissue perfusion) could be substantially restored. The first successful application of cardiopulmonary bypass in resuscitation was demonstrated by Kennedy in a case series in 1966, where seven of eight patients (who were otherwise refractory to conventional resuscitative measures) were successfully revived for a period of hours to days.22 Since then, VA-ECMO circuits have become smaller, more technologically sophisticated and widely available. This has facilitated its rapid growth in the management of cardiogenic shock and cardiac arrest. Indeed, the use of VA-ECMO for eCPR has surpassed 2,000 cases annually.23
Although use of eCPR for IHCA and OHCA have similarities in terms of rationale, technique, and logistics, there are important differences regarding patient selection. In patients with IHCA, underlying conditions are known and there is a higher frequency of potentially reversible etiologies. This is seldom the case for OHCA, although presentation with a shockable rhythm is often associated with an acute coronary syndrome that might be amenable to revascularization. Fewer trial data inform the use of eCPR for IHCA than for OHCA. For these reasons, we have confined this debate to use of eCPR for OHCA.
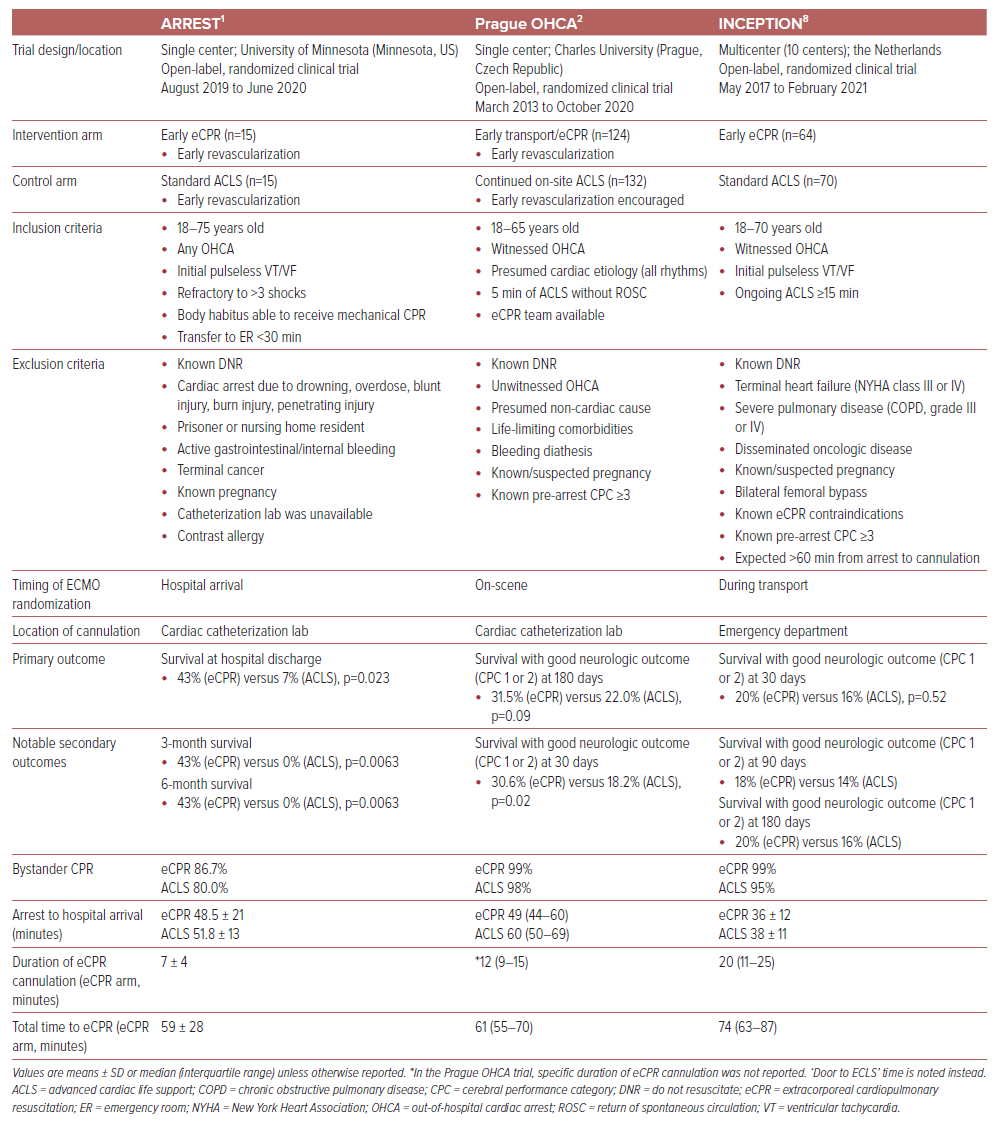
Despite the exponential increase in the use of eCPR, its role in clinical practice is uncertain. There have been conflicting results among three major trials for survival in patients with OHCA (Table 1).1,2,8,24 As delineated above, whether outcome differences can be attributed to differences in patient selection and the extent to which results across different trials can be combined remains debatable. Uncertainty about patient selection complicates assessments of cost-effectiveness as it is unlikely that an intervention will be cost-effective if not confined to the patients most likely to benefit. Finally, the degree to which results in dedicated centers of excellence can be extrapolated and eCPR capability incorporated in systems of care is uncertain.
One additional, and incompletely explored consequence of broader eCPR adoption would be the potential availability of organs for donation. This has particularly important relevance given the imbalance of patients awaiting organ transplantation and availability. While on the one hand, infrastructural requirements, logistical considerations and patient eligibility would already be delineated with an eCPR program, numerous other questions remain, including cost-effectiveness (although organ donation is generally considered cost-effective given the sparing of long-term medical costs), how best to effectively address withdrawal of care for eCPR patients, and long-term function of transplanted organs from this cohort.25
While a variety of questions remain, there is none bigger than how future trials should be designed. One could argue more efficacy trials are needed, as only one small study at one center has successfully met its primary endpoint. Whether future studies attempt to replicate ARREST precisely or not, they would need to be conducted in a network that is already set up to randomize and cannulate patients for eCPR rapidly and effectively. Inclusion criteria should be limited to those with the most potential to benefit (e.g. shockable rhythms, bystander CPR, minimized low-flow times). If successful, those trials could further strengthen the argument in favor of eCPR, and turn subsequent attention towards refining inclusion criteria, post-cannulation care protocols, or maintenance training for eCPR teams and networks. Conversely, if there is a consensus that the data for eCPR as an intervention are currently sufficient, an argument could be made to focus further efforts on effectiveness trials. These would expand eCPR to broader networks and delineate programmatic, logistical, and technical challenges with eCPR, as well as patient selection. Regional differences would come into play in the design of those trials as well. Given the intricacies of enrolling such hyperacute patients, the challenge of building eCPR programs, and the continuous evolution of standard of care in CPR, adaptive platform trial designs may be well suited to provide flexibility in treatment allocation ratios, factorial designs to permit testing of multiple strategies, and to adjust the study populations and interventions as data accrue.
Other complexities regarding the role of eCPR in cardiopulmonary arrest will need to be investigated as well. Although multiple patient factors have been associated with worse outcomes (such as medical comorbidities, older age, non-shockable rhythms on presentation, and higher lactate levels), there are numerous other inputs that are difficult to account for or regulate, including the quality of conventional CPR performed, time to bystander CPR (if done at all) and post-cannulation management.20,26,27 Moreover, ‘cardiac arrest patients’ have multiple different phenotypic profiles whose impact on outcomes have yet to be fully delineated. For example, there is now a greater appreciation of differences among hemodynamic profiles and treatment responses of cardiogenic shock secondary to acute MI (AMI-CS) versus that of heart failure (HF-CS). It is particularly difficult to sort this out during a cardiac arrest, although to some extent shockable rhythms are a proxy for the potential for reversible etiologies. Perhaps this too will evolve in patients who require CPR, allowing further ability to select appropriate eCPR candidates.
More broadly, the success or failure of eCPR as an intervention is highly dependent on logistical planning, procedural expertise, and post-cannulation management. In all three major trials comparing eCPR with conventional CPR, a transition to mechanical CPR and diversion to an appropriate center for cannulation was instituted.28 Widespread adoption of this resuscitative technique would require considerable coordination and knowledge of the healthcare framework in each region, with the incorporation and integration of EMS representing a critical component to its success. Moreover, higher volume centers and experienced operators tend to initiate VA-ECMO more rapidly, with lower complication rates.29 Whether eCPR should be initiated in the field (and if so, when), at an eCPR capable institution, or at a ‘spoke’ hospital with stabilization and subsequent transfer to a ‘hub,’ and who should cannulate is not fully clear. The best answer may vary in different settings, but this poses challenges for both trial design and extrapolation of trial results to broader application.
Regardless of which trial design will be selected, eCPR will have good results only if it is performed on a baseline of bystander CPR and rapid EMS response times. While EMS averages approximately 7 minutes after activation of 911 to arrival at the scene, these times rise dramatically in rural and low-income neighborhoods.30,31 Moreover, despite almost doubling the rates of survival when added to conventional CPR, only 40.2% of patients receive bystander CPR.18,32 As such, resources need to be channeled into improving basic CPR skills and increasing availability of automated external defibrillators (AEDs), especially in underserved areas. While we certainly need more information about how best to use new advanced technology therapies such as eCPR, we also need to continue to improve our implementation of proven resuscitative strategies.










