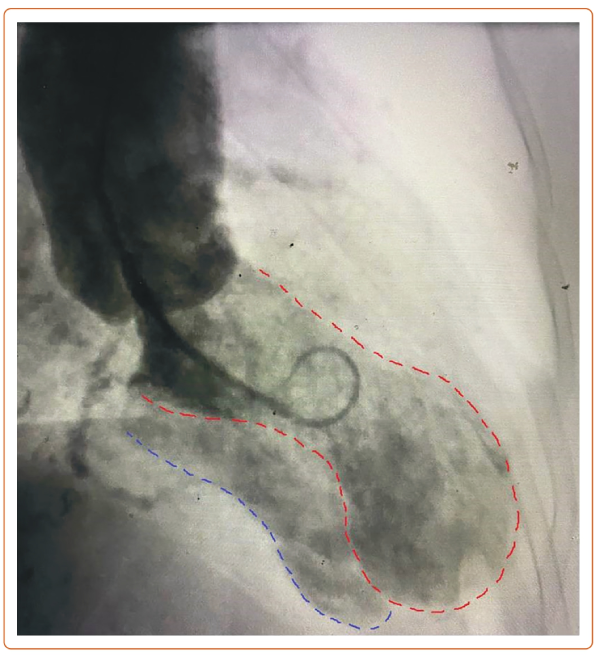
An 83-year-old woman presented with a 2-hour history of chest pain. She was not in acute distress. Exam showed a blood pressure of 128/98 mmHg, heart rate of 94 BPM and a grade 3/6 harsh systolic murmur. Troponin-I was 0.1 ng/ml. ECG showed ST-segment elevation in leads V2–V4 (Supplementary Figure 1). Emergency angiography showed a 95% stenosis in the left anterior descending artery and a 60% stenosis in the distal left circumflex artery and right coronary artery (Supplementary Video 1). Given the murmur on examination, a left ventriculogram was obtained, showing an apical aneurysm with opacification of the right ventricle and pulmonary artery consistent with a ventricular septal rupture (VSR; Figure 1 and Supplementary Video 2). An oximetry run showed a 19% step-up in oxygen saturation from the right atrium to the right ventricle. Echocardiogram confirmed the diagnosis of a VSR, measuring 7 mm in the apical inferior septum with left-to-right shunt (Supplementary Video 3 and Supplementary Figure 2). Given the absence of ongoing chest pain and the presence of Thrombolysis in MI III flow in the left anterior descending artery, the patient was initially treated conservatively and later referred for coronary artery bypass grafting and VSR repair.
This case highlights the variable time to VSR in ST-segment elevation MI. Traditionally VSR was considered to be a late complication, however, it can occur at 5–24 hours after symptom onset.1–3 Diagnosis is challenging in early cases when there is clinical and hemodynamic stability. In such cases it is critical to recognize subtle signs, such as a heart murmur, and consider the use of a ventriculogram, which may aid in timely diagnosis. 










