In late December 2019, an outbreak of an unknown disease called a pneumonia of uncertain cause occurred in Wuhan, Hubei Province, China.1 Over the next few days, several independent laboratories identified the causative agent as a novel coronavirus.2–4 The WHO has temporarily named this virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the related infectious disease coronavirus disease 2019 (COVID-19). According to the WHO’s daily report, there were 332,930 cases globally as of March 23, 2020, and there have been 14,509 deaths. The COVID-19 epidemic has evolved into a global health crisis.
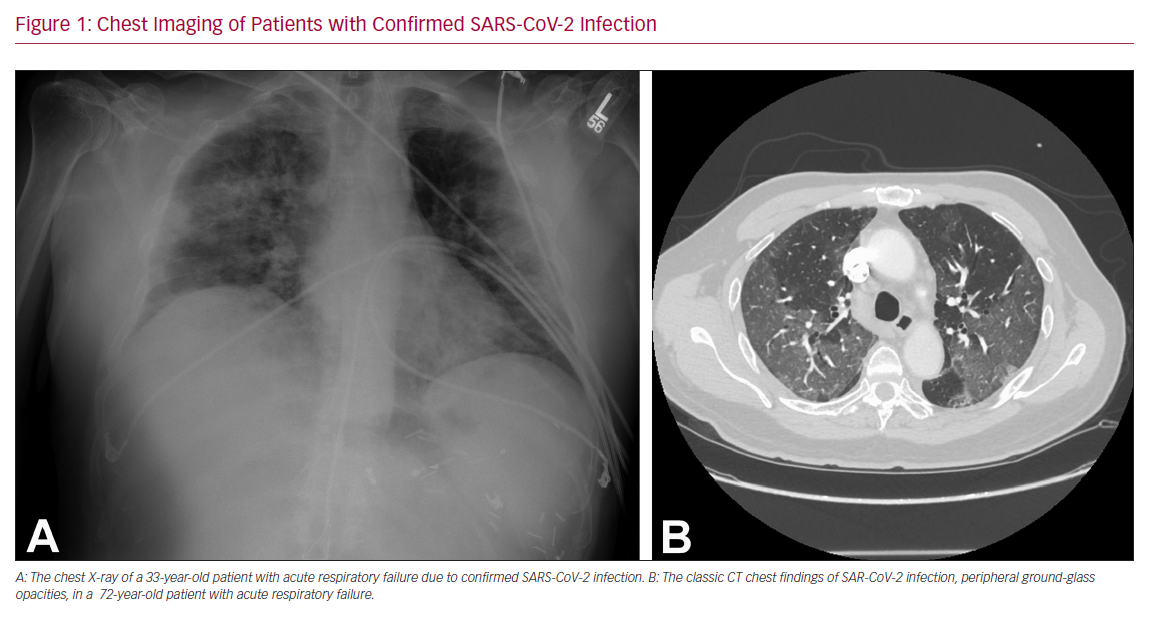
The main reported symptoms of COVID-19 are fever (77–98%), fatigue (52–75%), and cough (60–81%).5–7 While it predominantly affects the respiratory system (Figure 1), SARS-CoV-2 has also been shown to affect other organ systems, including the gastrointestinal and cardiovascular systems. COVID-19 is only a few months old, and hence a lot remains unknown, but it appears that patients with cardiovascular disease (CVD) are among those with the highest risk for mortality and morbidity, along with the elderly. In a case series of 21 patients with COVID-19 requiring intensive care unit (ICU) level care in Washington State, congestive heart failure was the second most common baseline co-morbidity (42.9%), behind chronic kidney disease (47.6%).8
The purpose of this article is primarily to summarize the available literature on how this novel disease affects the cardiovascular system, especially in patients with pre-existing cardiovascular co-morbidities.
Cardiac Complications
Published and anecdotal reports suggest that acute-onset heart failure, arrhythmias, acute cardiac injury including MI, myocarditis and cardiac arrest are among potential cardiovascular complications of COVID-19.5–7 It is likely that the pro-inflammatory state induced by this viral infection, and subsequently increased metabolic demand, lead to several of the aforementioned cardiac complications.
This has been well-established in patients with influenza infection and appears to be the case in those with SARS-COV-2 as well.9 There remains a paucity of data on whether the risk of cardiac complications is higher among patients with pre-existing cardiovascular co-morbidities compared with their CVD-naïve counterparts.
Cardiac Biomarkers and Acute Cardiac Injury
In the recently published retrospective study of 191 COVID-19 patients from two separate hospitals in China, the incidence of elevation in high-sensitivity cardiac troponin I (cTnI) (>28 pg/ml) was 17%, and it was significantly higher among non-survivors (46% versus 1%, p<0.001).10 Furthermore, elevation of this biomarker was noted to be a predictor of in-hospital death (univariable OR 80.07, 95% CI [10.34–620.36], p<0.0001). The most abrupt increase in cTnI in non-survivors was noted beyond day 16 after the onset of disease. In the same study, the incidence of acute cardiac injury was 17% among all-comers, but significantly higher among non-survivors (59% versus 1%, p<0.0001).
Another study reported the incidence of acute cardiac injury to be 7% (10 out of 138 patients), but significantly higher among patients requiring ICU care (22.2% versus 2%, p<0.001).6 A meta-analysis of cardiac biomarkers in COVID-19 patients showed that the values of cardiac troponin I were significantly higher in patients with severe disease than in those without (standardized mean difference 25.6 ng/l; 95% CI [6.8–44.5]).11 Most patients with COVID-19 only have a mild elevation in cTnI, and values exceeding the 99th percentile of the upper reference limit can only be seen in 8–12% of positive cases.12 However, it appears that the magnitude of cTnI seems to be highest among patients with most severe disease. Hence, it is reasonable to suggest that initial measurement of cardiac biomarkers at the time of hospitalization, as well as longitudinal monitoring during the hospital stay, may help identify a subset of patients with evidence of acute cardiac injury and worse prognosis. Of note, in a case series of 140 COVID-19 patients from Wuhan, China, only a few (6.7%) patients had increased serum level of creatinine kinase, and there was no difference based on disease severity.5
The exact etiology of elevation in cardiac biomarkers among these patients has not been reported, but we must be cautious not to chalk it up to demand ischemia, because acute myocarditis and acute coronary syndromes (ACS) may also be potential causes. In fact, the angiotensin-converting enzyme 2 (ACE2) receptor, the binding point for SARS-CoV-2 is abundantly found in myocytes, and hence myocyte damage from a direct viral attack could very well be the predominant mechanism. A comprehensive work-up to identify the exact etiology of elevated biomarkers may not always be possible, especially in critically ill patients.
Furthermore, we shall have to balance the risks and benefits of pursuing invasive and noninvasive testing that could potentially expose providers and contaminate equipment, especially given the contagious nature of this illness, and the ability of this virus to survive on surfaces for multiple days. A recent study showed that the median half-life of SARS-CoV-2 is 5.6 hours on stainless steel and 6.8 hours on plastic.13 In patients with suspected ACS as the etiology of elevated cardiac biomarkers, thrombolytics may be a valuable alternative treatment to primary percutaneous coronary intervention to minimize contamination of the catheterization laboratory.
Cardiac Arrhythmias
In one of the earliest retrospective reviews of COVID-19 patients treated in China, Wang et al. found that of the 138 patients analyzed, 23 (17%) had cardiac arrhythmias and the incidence was significantly higher among those requiring ICU care (44.4% versus 6.9%, p<0.001), compared with those treated in non-ICU beds.6 The authors did not specify if these arrhythmias were atrial or ventricular or their median duration.
Another study reported that cardiac arrhythmias were significantly more common in patients with critical forms of COVID-19 than in mild and moderate cases.14 Telemetry monitoring for arrhythmias might be reasonable for all COVID-19 patients but especially recommended for those with pre-existing CVD, elevation in cardiac biomarkers, or with severe forms of COVID-19. In the absence of any evidence to the contrary, arrhythmias in COVID-19 patients should be treated with anti-arrhythmic drugs in the same manner as non-COVID-19 patients. In fact, amiodarone has been shown to inhibit in vitro spreading of SARS coronavirus. Extrapolating from this data, some experts recommend administration of prophylactic intravenous amiodarone to mitigate the risk of late sudden cardiac arrest among patients infected with the novel SARS-COV-2.15
Myocarditis
The exact incidence of COVID-19-related myocarditis is currently unknown. However, the pathogenicity of SARS-CoV-2 is similar to the Middle East respiratory syndrome coronavirus (MERS-CoV), which has been shown to cause acute myocarditis and heart failure.16 Hence, it is reasonable to hypothesize that as our understanding and reporting of SARS-CoV-2-related adverse cardiovascular events evolves, we can expect to see increasing cases of COVID-19-related acute myocarditis.
Elevated cardiac biomarkers, new-onset cardiac arrhythmias, and acute-onset heart failure symptoms in a SARS-CoV-2 patient should raise clinical suspicion for acute myocarditis. At the current time, the clinical utility of endomyocardial biopsy in confirming the diagnosis remains unclear. Non-invasive imaging such as cardiac PET or cardiac MRI to evaluate for myocardial inflammation might be helpful in cases of diagnostic uncertainty, if they can be performed with adequate isolation precautions.
In a recent report of a 37-year-old patient with SARS-CoV-2-related fulminant myocarditis, Hu et al. showed successful treatment with a combination of methylprednisolone (200 mg/day, 4 days) and immunoglobulin (20 g/day, 4 days).17 Studies have shown that one of the most important mechanisms of clinical deterioration in COVID-19 is from a cytokine storm.18,19 This may explain why high-dose steroids may be effective in the treatment of fulminant myocarditis caused by this novel virus. There are some anecdotal reports of utilizing plasmapheresis and the extracorporeal cytokine absorber CytoSorb (CytoSorbents) in combating the cytokine storm, although there are no published studies on this as yet.
Acute Heart Failure and Cardiogenic Shock
In one case series of COVID-19 patients, the incidence of acute heart failure was 23% (44 out of 191 patients) and significantly higher among non-survivors (52% versus 21%, p<0.0001).10 Multiple precipitating etiologies, including acute coronary syndrome, cardiac arrhythmias, stress-induced cardiomyopathy, and fulminant myocarditis, might result in acute heart failure or cardiogenic shock in this patient population. Coronary CT angiogram and echocardiography may provide valuable non-invasive diagnostic evaluation that may be critical in guiding further therapies. The clinical threshold to obtain these tests should be low, especially a formal or bedside echocardiography in patients with severe COVID-19. Pulmonary artery catheters might be extremely useful tools for diagnosis and to guide therapy in these complex patients who are most likely to be suffering from mixed cardiogenic and vasodilatory shock, although the evidence is currently lacking for their use.
Investigational Therapies and Cardiac Concerns
Anti-viral Drugs
The combination of lopinavir and ritonavir (Kaletra, AbbVie) is a well-established antiretroviral therapy for HIV/AIDS. It was reported to have the potential to treat SARS infections, and hence has been thought to be useful in the treatment of SARS-CoV-2 virus as well.20 In a case series of 62 COVID-19 patients published by Xu et al., 46 patients received lopinavir/ritonavir therapy, either alone or in conjunction with other therapies; one patient had been discharged from the hospital and no patients had died at the time of the publication.7 This combination was also a part of the treatment algorithm in the treatment of COVID-19 patients in at least one other case series from China.10 However, in a recently published open label randomized controlled trial comparing lopinavir/ritonavir (400 mg and 100 mg respectively) versus standard care in COVID-19 patients, the former was found to be no better.21 Oseltamivir is another antiviral that has been used in the treatment of SARS-CoV-2.6
One of the known adverse cardiac effects of lopinavir/ritonavir is hyperlipidemia (hypertriglyceridemia and hypercholesterolemia). In 2009, the US Food and Drug Administration warned about the potential of this drug to prolong QT and PR intervals, and recommended that caution be exercised when prescribing it in patients with structural heart disease. Therefore, patients being treated with this therapy for COVID-19 should undergo close cardiac monitoring, especially if they have pre-existing cardiac co-morbidities or develop them during the course of their illness. Oseltamivir is fairly cardio-benign, and in fact in animal models has been shown to reduce the risk of atrial and ventricular arrhythmias.22,23
Anti-malarial Drugs
Chloroquine, a widely used anti-malarial and autoimmune disease drug, has recently been reported as a potential broad-spectrum anti-viral drug.24,25 Chloroquine is known to block virus infection by increasing the endosomal pH required for virus/cell fusion and interfering with the glycosylation of cellular receptors of SARS-CoV.26 Hydroxychloroquine has the same mechanism of action as chloroquine, but its more tolerable safety profile makes it the preferred option. In a recent study examining the pharmacological activity of chloroquine and hydroxychloroquine, both drugs were tested using SARS-CoV2-infected Vero cells.27 In this laboratory study, hydroxychloroquine was found to be more potent than chloroquine at inhibiting SARS-CoV-2 in vitro. Based on these findings, the authors of the study propose an off-label use of hydroxychloroquine sulfate to treat SARS-CoV-2 infection. They suggest a loading dose of 400 mg twice daily for the first day, followed by a maintenance dose of 200 mg twice daily for 4 days.
Hydroxychloroquine-related cardiac adverse events are rare, but can be severe and occasionally life-threatening. A recent review of cardiac complications attributed to this medication found that most patients who developed cardiac symptoms had been on treatment for a long period of time (median 7 years), and had been exposed to large cumulative doses (median 1,235 g).28 The most common adverse event was conduction abnormalities (prolonged QT and PR intervals), which affected 85% of these patients. Although it appears that conduction abnormalities are a long-term sequela of high-dose and prolonged use of hydroxychloroquine, we recommend monitoring COVID-19 patients being treated with this drug for cardiac arrhythmias.
Angiotensin-converting Enzyme Inhibitors and Angiotensin Receptor Blockers
There has been a tremendous amount of speculation surrounding the potential adverse effects of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) in COVID-19 patients. Numerous social media posts have suggested that these commonly used drugs may not only increase the risk of infection, but also the severity of COVID-19.
The concern arises from the observation that, like the coronavirus causing SARS, the SARS-CoV-2 virus binds to a specific receptor called ACE2 to infect cells, and ACE2 levels are increased following treatment with ACEIs and ARBs.29 However, any concerns regarding the safety of these drugs in COVID-19 patients lacks sound scientific evidence. In fact, there is evidence that ACEIs may be protective against viral pneumonias.30–32 Similarly, there have been studies in animals infected with SARS-CoV-2 where these medications have been shown to be protective against serious lung complications, but to date human data are lacking.33 Hence, we recommend that physicians and patients continue their treatments with ACEIs and ARBs because there is no clinical or scientific evidence that they cause or worsen COVID-19 infection. The European Society of Cardiology’s Council on Hypertension also recommends likewise in its recent position statement.33
Extracorporeal Membrane Oxygenation
Veno-arterial (VA) and veno-venous (VV) extracorporeal membrane oxygenation (ECMO) may both be extremely valuable in treatment of COVID-19 patients suffering from refractory cardiac and respiratory failure, respectively. Approximately 15–30% of COVID-19 patients develop acute respiratory distress syndrome (ARDS).6,34 ECMO has been used in some patients with COVID-19 and ARDS in China, but detailed characteristics of these patients remain unknown at this time.6 The WHO interim guidelines make general recommendations that patients in severe refractory ARDS should be referred to centers capable of providing ECMO support.35 Generally, criteria for initiation of VV and VA ECMO in COVID-19 patients are the same as for non-COVID-19 patients. The chief concern is protection of personnel involved in the implantation of ECMO. Anecdotal reports from South Korea, Japan, Italy and China have all shown mixed outcomes among patients initiated on ECMO, most likely owing to the severity of their disease necessitating treatment of ECMO.
There is an ongoing ELSOCard registry study looking at outcomes on ECMO among COVID-19 patients, which shall be very telling. In the meantime, it is crucial to appreciate that ECMO is a resource-intensive, highly specialized, and expensive form of life support with the potential of significant complications, and hence should only be reserved for truly refractory cases. It is a finite resource, and must be used judiciously, especially in the midst of a pandemic where all resources are stretched thin.
Strategies to Minimize Potential Patient Exposure
Much still remains unknown about the natural history of this novel virus. Hence, the cliché of prevention is better than cure is true now more than ever. All the case series published to date have confirmed that patients with pre-existing cardiovascular co-morbidities have a higher risk of mortality with COVID-19.5–7 It is paramount that all measures to minimize patient exposure to SARS-CoV-2 be implemented broadly and effectively, including social distancing, proper hand hygiene and cancellation of elective clinic and hospital visits.
As is eloquently discussed in a recent editorial by Dr Lisa Rosenbaum, we must learn from the tragedy in Italy to prevent our medical system in the US from being overwhelmed, and so we are not forced to make the heartbreaking decisions facing Italian providers.36 Indeed, as she says, the “best outcome of this pandemic would be being accused of having over prepared”.
Heart Transplantation
One area of cardiovascular medicine that remains especially vulnerable in such pandemics is that of heart transplantation. Patients who are recipients of orthotopic heart transplantation, and those awaiting transplants are both at risk. The eminent risk for the former is more obvious owing to their immunocompromised state.
In an attempt to mitigate this risk, our institutions have instituted strict policies for COVID-19-suspected or confirmed patients to not be admitted in ICUs shared with our transplant patients.
A recently published survey of 87 heart transplant recipients during December 20, 2019 and February 25, 2020 in China showed that these patients had a low rate of infection with SARS-CoV-2, and transition to COVID-19, as long as they practiced social distancing.37 Only four patients had upper airway infections and three of them tested negative for SARS-CoV-2; the fourth patient recovered well and did not need any testing.
The safety of patients awaiting heart transplantation has also been jeopardized by the COVID-19 pandemic due to potential transmission from the donor to the recipient. We know too little about this novel virus to reliably estimate the risk of transmission through donor organs. Furthermore, until rapid testing for SARS-CoV-2 becomes readily available, there will be no way to definitively confirm negative status of the donor in a timely manner. It is reasonable to hypothesize that we may see a surge in implantations of durable left ventricular assist devices as bridge to transplantation until our understanding of the risk of transmission is more robust, or we have a definitive treatment for this novel virus, or until this pandemic has passed.
Conclusion
Our knowledge of the novel coronavirus and its cardiovascular implications is evolving by the hour. It is critical that, as a medical community which is on the front lines of this pandemic, we share our experiences, the successes, and the failures, with one another at a rapid pace. In addition to published manuscripts, real-time anecdotal experiences shared by world experts on social media forums will remain a valuable tool as we continue to learn about this disease.