Chest pain is one of the most common reasons for an emergency room (ER) visit in the US with almost 6 million ER visits annually.1
According to the fourth universal definition of MI, acute MI (AMI) requires a rise and/or fall in cardiac troponin (cTn) with at least one value above the 99th percentile upper reference limit.2,3 Cardiac troponin I (cTnI) and cardiac troponin T (cTnT) are the preferred biomarkers in acute coronary syndrome (ACS).2–5
Although contemporary cTn assays are used routinely in the US for risk stratification and the diagnosis of patients presenting with suspected ACS, they have important limitations compared to high-sensitivity cardiac troponin (hscTn) assays:
- They are highly imprecise: most contemporary assays have a total imprecision (coefficient of variation) of 10–20% at the 99th percentile for the diagnosis of AMI.
- They have limited analytical sensitivity: contemporary assays can only quantify cTn in <35% of healthy individuals below the 99th percentile.4
These limitations have led to prolonged serial sampling protocols being used to achieve optimal diagnostic accuracy, which mean increases in hospitalizations, length of stay, and costs.4,6–10
In conventional troponin assays, troponin elevation is considered to be an all or nothing phenomenon. The presence of troponin elevation above the 99th percentile reference range suggests myocardial injury but no troponin elevation above the 99th percentile is considered normal, even though this does not necessarily mean the absence of an ACS, as conventional assays are unable to detect small ischemic events. Particularly where there is atypical chest pain and no troponin elevation, patients who are experiencing an ACS are at risk of being discharged early because the decision-making process is subjective.9
To overcome this difficulty, hscTn assays were introduced and have slowly gained importance. These can be used to classify patients more appropriately as ‘true’ or ‘no’ ACS, and do not require repeat assays at 6 and 12 hours, unlike conventional cTn assays. HscTn assays are able to detect troponins at a concentration about 1/10 of the lower reference range of conventional troponin assays.2
While hscTn assays have been in clinical use since 2015 in Europe, the FDA only approved their use in the US in 2017.7 There is a lack of clarity on interpreting the results of hscTn assays, despite a decade of published studies, as they differ significantly from conventional troponin assays.10
This review discusses the basics of hscTn assays and their interpretation in patients presenting with symptoms suggestive of ACS.
Basics of Troponin Analysis in Acute Coronary Syndrome
CTnI and cTnT are contractile components present in the myocardium and are exclusive to cardiac muscles.2,3,11 They work in coordination with calcium ions to promote binding of actin and myosin, thus promoting cardiac muscle contraction. CTn consists of troponin T (protein molecule attaching troponin complex to actin), troponin C (calcium binding site) and troponin I (inhibits myosin head interaction in the absence of calcium). While troponin C can be found in both skeletal and cardiac muscles, troponin T and I are specific and sensitive, so are called cardiac-specific troponins.
It is important to understand the concept of the ‘early releasable troponin pool’ (ERTP). Almost 95% of troponin is bound to actin filaments while about 5% of it is free in the cytoplasm, which constitutes the ERTP.12 The troponin in the ERTP is the first to be released following any myocardial injury but, with normal renal function, gets cleared immediately from the blood pool. The structurally bound troponin, on the other hand, is released over a period of several days, causing a gradual rise in troponin. The half-life of cTn is around 2 hours.
Common Definitions of Clinical Importance
While using hscTn assays, interpreting the values requires an in-depth understanding of a few definitions. The precision of the hscTn assay is defined by the coefficient of variation (CoV). This is the ratio of standard deviation to the mean value of a series of troponin samples. Generally, hscTn assays are approved for use per guidelines if their CoV is <10% at the 99th percentile. If the CoV is 10–20%, the test can still be used but tests that have CoV >20% are not acceptable for clinical use.
Limit of blank (LoB) is the highest concentration of troponin reported by a hscTn assay when there is no troponin in the sample. Limit of detection (LoD) refers to the lowest possible concentration of troponin that can reliably be differentiated from LoB. Limit of quantification (LoQ) refers to the lowest troponin concentration reported by a particular laboratory, and this may or may not correlate with LoD. Delta refers to a clinically significant change in troponin levels measured over fixed intervals which is used to identify myocardial injury, even if troponins are in the <99th percentile. The hscTn assays analyze troponin as a continuous variable, rather than a fixed value.
What is High Sensitivity?
An hscTn assay should be able to detect low concentrations of troponins and should have high sensitivity and precision. The Internal Federation of Clinical Chemistry (IFCC) Task Force on Cardiac Bio-Markers defines hscTn assays as: having a total imprecision (CoV) ≤10% at the 99th percentile; and being able to measure cTn above the LoD in ≥50% of healthy subjects.4,13 The hscTn assays have increased analytical sensitivity and reduced variability, which facilitates integration into clinical pathways.7
Therefore, hscTn assays should be able to measure troponins consistently and accurately in a majority of healthy individuals (who have very low concentrations) with negligible variability. Multiple factors affect hscTn assay results, including age, sex, standardization of methods and specimen type, and these should be considered while reporting absolute values. As an example, men usually have a slightly higher value than women.6,13 Also, patients aged over 60 years have relatively higher troponin at baseline.14 The IFCC recommends establishing the 99th percentile for any particular assay using appropriate statistical power, which requires a minimum of 300 male and 300 female patients.
What do the Guidelines Say?
The IFCC guidelines recommend hscTn assays because of their ability to measure cTn values above the assay’s LoD in more than 50% of individuals.6,13 The 2015 European Society of Cardiology (ESC) guidelines give a class I indication for use of both the rapid 0/1-hour rule-out and rule-in protocols and the 0/3-hour protocol.7 The European algorithm allows triage in about 75% of patients. It is important to remember that all troponin assays are associated with some false positive and false negative results, but this is minimal with hscTn.
Approved High-sensitivity Troponin Assays
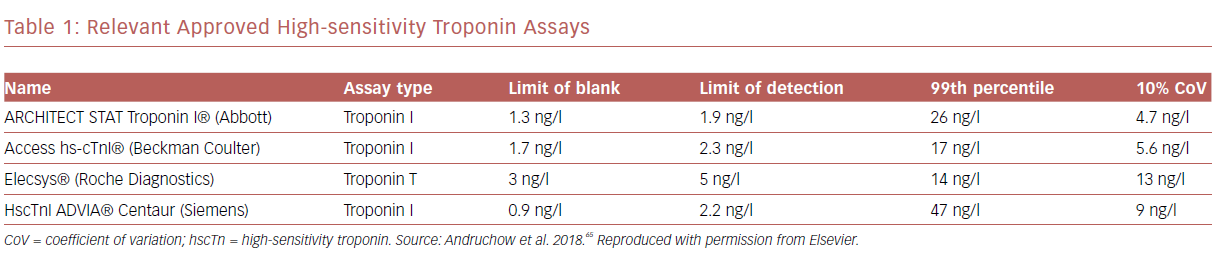
There are at least four hscTn assays that are approved and in clinical use. One of them measures troponin T (Elecsys®, Roche Diagnostics) and the other three assays measure troponin I (ARCHITECT STAT troponin I, Abbott; Access hs-cTnI, Beckman Coulter; hs-cTnI ADVIA Centaur, Siemens). The reference ranges for each of the individual tests is shown in Table 1.
Algorithms Using High-sensitivity Troponin Assays
At least four protocols are worth discussing:
- rule-out strategies using hscTn;
- accelerated protocol with serial repeat hscTn assays for rule-out/rule-in;
- hscTn combined with risk scores; and
- single hscTn measurement.
Rule-out Strategies Using hscTn: Absent Troponin at Presentation
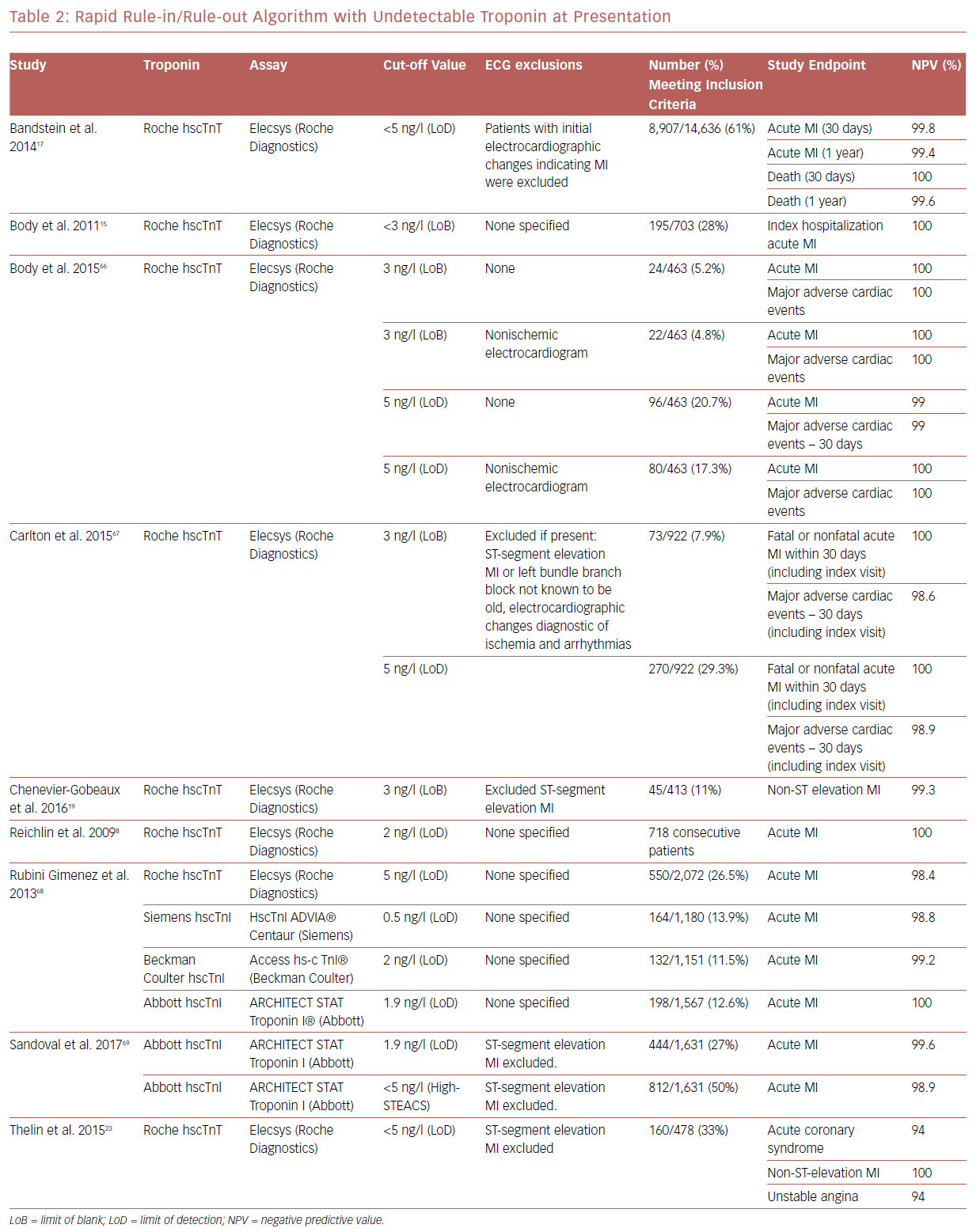
As hscTn assays measure very low troponin values, it makes sense that a one-time troponin assay should be able to exclude ACS with a very high clinical diagnostic accuracy (negative predictive value). A number of studies have shown that a low concentration of troponin levels using hscTn assays, below the LoD or LoB, has a very high negative predictive value (Table 2).15–20 Troponin levels lower than LoD values can exclude ACS with >99% confidence according to published meta-analyses.21,22 However, unstable angina cannot be ruled out with this approach.23 The FDA does not allow reporting troponin levels below 6 ng/dl, which is greater than both the LoD and the LoB for the Roche hscTn assay. This technically prevents patients being discharged from ED on the basis of on a single low concentration hscTn and opinions on this issue have been mixed.24 Of note, low troponin values below the LoD may have a lower sensitivity, so the ESC guidelines recommend re-testing >3-hour symptom onset before presentation when troponin values are less than the LoD.25 There are a few unanswered questions with this approach including: should the test be done on all patients or only those with non-ischemic EKGs? Should LoB or LoD be used? Will the test maintain CoV <10% at such low level troponins?
Accelerated Protocol with Serial Repeat hscTn Assays for Rule-in/Rule-out
Most centers in the US use longer troponin rule-out algorithms.26,27 However, the 2015 ESC guidelines give a class I recommendation for 0/1-hour hscTn protocol.7 A few 1- and 2-hour algorithms use hscTn.28–31 The presence of serial, dynamic hscTn promotes an early rule-in ACS with higher specificity whereas the absence of serial hscTn elevation promotes early rule-out ACS with high sensitivity.4,32,33 It is important to remember that dynamic troponin elevation does not confirm ACS as it could indicate MI. In addition, an absolute increase in troponin concentration has been shown to have a higher diagnostic accuracy than relative changes in troponins.34
High-sensitivity Cardiac Troponin with Risk Scores
A few studies have examined the use of EKG, hscTn, and clinical risk prediction scores at some centers.35–40 Most of these covered accelerated diagnostic protocols combining some risk scores, most commonly Thrombolysis in Myocardial Infarction (TIMI). Data on what would be the most appropriate risk score and the ideal troponin assay to use are still limited. Future studies testing combinations of various test scores with different hscTn assays are essential.
Single High-sensitivity Cardiac Troponin at Presentation
The concept of selecting a threshold for hscTn based on clinical need rather than the analytical ability of the test has been emerging recently, as shown in the High-Sensitivity Troponin in the Evaluation of Patients With Acute Coronary Syndrome (High-STEACS) study.41 The investigators did not use the LoD or LoB cut-offs, but rather they used a fixed cut-off of 5 ng/l to safely discharge patients with possible ACS. The study showed a negative predictive value of 99.6% for the primary outcome of index MI, subsequent MI, or early cardiac mortality.
Interpreting Elevated Troponin at Presentation
Any degree of troponin elevation, irrespective of etiology, is associated with a poor prognosis.42–45 That said, troponin values five times the normal have been shown to be associated with poor outcomes in ACS with an estimated positive predictive value of 90% and a specificity of >95%. Serial troponin rise is important to define MI, so stable elevated values over a period of time should be investigated for the presence of possible macrocomplexes, even while using hscTn assays.46
What is the Ideal Time to Repeat Troponin Assays?
In patients with symptoms suggestive of ACS, it is recommended that an initial troponin should be taken at presentation, followed by a second sample obtained at a fixed time interval between 1 and 3 hours. The idea behind obtaining a second troponin with the hscTn assay is to identify clinically significant changes in troponin levels, both relative and absolute. Since small relative changes in troponin elevations could be related to the analytical errors of the test itself, it is recommended that absolute rather than relative changes in troponin levels are used.47–49
A number of studies have compared the efficacy of 1-, 2-, and 3-hour repeat troponins. Studies have shown that 1- and 2-hour algorithms carry similar sensitivities of >96% and a negative predictive value of >99%, while the 3-hour algorithm appears to have a mildly lower sensitivity but similar negative predictive value.18,51–54 As 1-hour algorithms depend on a small rise in troponin concentration, this may carry a risk of missing an ACS. Therefore, the 2-hour repeat strategy seems to be the most reasonable approach, even though guidelines do not support one over the other. As mentioned above, using risk scores, including the Global Registry of Acute Coronary Events (GRACE) or History, ECG, Age, Risk factors and Troponin (HEART) score, along with the hscTn assay could help to improve the sensitivity of analysis. The HEART score seems to be preferred above other risk scores.55 Nevertheless, to avoid unsafe early discharges in patients with evolving ACS, it is essential to consider the overall picture including serial EKGs and risk assessment tools.
To summarize, there are at least six algorithms. The 0/3-hour algorithm from the European guidelines and the 2–hour advanced diagnostic pathway use risk score prediction tools whereas the 0/2-hour, 0/1-hour ESC, modified 0/1-hour ESC and the current US state-of-the-art algorithms (6- and 12-hour troponins) do not include risk prediction tools.
While implementing the early rule-in/rule-out algorithms, it is essential to make sure that the patient has had chest pains for at least 3 hours before presentation, or an evolving ACS may be missed, and an erroneous early discharge made.
While using these algorithms, patients should be involved in shared decision making, especially where there is a low likelihood of ACS and the patient cannot stay longer because of other reasons. In such cases, it is essential to advise the patient regarding the risks and to establish an outpatient follow-up within a reasonable amount of time.
Type I Versus Other Types of Myocardial Injury
An ideal troponin assay should not only identify a possible myocardial injury but also help practitioners to understand the pathophysiology of MI. Differentiating whether an MI is a true type I MI secondary to a plaque rupture causing a type I MI, or various other mimics of plaque rupture including but not limited to cardiomyopathy, myocarditis, pulmonary embolism with right heart strain, hypertensive emergency, coronary vasospasm, stress cardiomyopathy, or demand ischemia.56 Knowing this is important when deciding the next step in patient care and to avoid unnecessary investigations and anxiety.
Unfortunately, most troponin assays, including hscTn, cannot be used to differentiate between different types of MI using one absolute value. This could be related to the various cut-off values for the different algorithms and so practitioners are left with to depend on serial troponin (whether a 1-hour or 6-hour repeat) and serial EKG changes. Even in the current era of hscTn, differentiating between various types of MIs continues to be a challenge. However, hscTn has be shown to diagnose fewer MIs than conventional troponins, so is less likely to give false-positive results for other types of MI.57
The Indeterminate Grey Zone
A limitation of using hscTn is there is a subgroup of patients who clearly do not fit into the rule-in or the rule-out algorithms. About 15–40% of patients fall into an indeterminate grey zone.30,50,58,59 These patients have an intermediate to a high risk of having a cardiac event, including death, with an ACS incidence of 5–20%.30,50,52,58,59 The ESC guidance document recommends using clinical judgement while dealing with patients in this grey zone.60
This focuses on patients:
- who experience typical symptoms but have hscTn less than the 99th percentile;
- who experience typical symptoms with hscTn less than the 99th percentile but at least above LoD;
- who experience typical symptoms with hscTn greater than the 99th percentile but without any dynamic change in levels during repetition; and
- who experience typical symptoms with hscTn greater than the 99th percentile and with dynamic change in the levels during repetition but without any acute coronary pathology including rupture, erosion or dissection.
This involves reviewing previous medical records for chronic hscTn elevations, performing serial EKGs, repeating hscTn at a fixed time interval, and using a risk prediction tool (preferably the HEART score). This helps to classify patients who fall into this grey zone as low, intermediate and high risk.
Age- and Sex-specific Algorithms
At least four clinical variables correlate with outcomes in patients with ACS including age, sex, time of chest pain onset and renal dysfunction. Three algorithms have been proposed. The first incorporates all four parameters, but is not commonly used. The second algorithm uses sex-specific cut-offs but does not account for renal dysfunction and age; this is because previous studies have shown that women presenting with ACS are older than men by almost 5–8 years on average.61–63 Female sex is usually associated with relatively lower troponin, but the age factor compensates well for the troponin difference without the need for using age-adjusted cut-off values (the higher age in women increases their troponin levels and corrects the age difference). However, using only sex-specific cut-off values reclassifies only a few patients into a different risk category compared to uniform cut-off criteria.61,64 The third model, recommended by the ESC guidelines, uses uniform cut-off values for all patients without accounting for age, sex, or renal function.7 Further research on the effect of these confounder variables on hscTn assays is essential.
Conclusion
HscTn is clearly a significant advance in the early and accurate diagnosis of ACS and has the potential to improve patient outcomes through early, appropriate evidence-based interventions.
In patients who do not have ACS, it helps to rule out MI and helps to discharge patients early, thus reducing patient anxiety, unnecessary admissions and costs.
It is important to understand how to interpret hscTn results because they differ from conventional troponin assays. In addition, there is an intermediate zone where it is difficult to rule in or rule out MI. Until further evidence becomes available, clinicians should combine hscTn with appropriate risk prediction tools.
The importance of shared decision making and clinical judgement should never be underestimated.